
AN INTRODUCTION TO ANAESTHESIA
This booklet aims to offer you, your relatives and friends an introduction to anaesthesia. There are wide differences in how much information people want. Only you can know how much you want to know. We offer some information here and suggest how and where you can find out more.
Your anaesthetist will discuss the anaesthetic methods that are appropriate for you and will find out what you would like. Sometimes you can make choices if you want to – anaesthetists try to offer individual care. You and your anaesthetist can work together to make your experience as calm and free from pain as possible.
What is anaesthesia?
The word anaesthesia means loss of sensation. If you have ever had a dental injection in your mouth or pain-killing drops put in your eyes, you already know important things about anaesthesia.
- It stops you feeling pain and other sensations.
- It can be given in various ways.
- Not all anaesthesia makes you unconscious.
- It can be directed to different parts of the body.
Drugs that cause anaesthesia work by blocking the signals that pass along your nerves to your brain. When the drugs wear off, you start to feel normal sensations again, including pain.
SOME TYPES OF ANAESTHESIA
Local anaesthesia
A local anaesthetic numbs a small part of your body. It is used when the nerves can easily be reached by drops, sprays, ointments or injections. You stay conscious but free from pain.
Regional anaesthesia
Regional anaesthesia can be used for operations on larger or deeper parts of the body. Local anaesthetic drugs are injected near to the bundles of nerves which carry signals from that area of the body to the brain. There are 2 types of regional anaesthesia:
- Spinal and epidural anaesthesia in which a local anaesthetic is injected near the spinal cord and nerve roots. It blocks pain from an entire region of the body, such as the belly, the hips, the legs, or the pelvis. Epidural and spinal anaesthesia are used mainly for surgery of the lower belly and the legs. Epidural anaesthesia is often used in childbirth. You will remain conscious but free from pain;
- Peripheral nerve block in which a local anaesthetic is injected near a nerve or group of nerves that supply the part of your body being operated on. It provides long-lasting pain relief, during and after surgery, that can last from 2 to 18 hours, depending on the injection site and which medicines are used, and can be repeated. A nerve block can be used for surgery on the shoulder, elbow, forearm, wrist, hand, fingers, knee, leg, ankle, or foot, and also for some procedures on thorax and abdomen.
When regional anaesthesia is feasible, there are many advantages to perform it, either as a stand-alone procedure or combined with general anaesthesia.
Sedation
Sedation is the use of small amounts of anaesthetic or similar drugs to produce a ‘sleepy-like’ state. It makes you physically and mentally relaxed during an investigation or procedure which may be unpleasant or painful (such as an endoscopy). You may remember a little about what happened or you may remember nothing. Sedation may be used by other healthcare professionals as well as anaesthetists.
Combining types of anaesthesia
Anaesthetic drugs and techniques are often combined.
When the length of the procedure is expected to be long or the positioning on the operating table uncomfortable, general anaesthesia or sedation is administered to make you comfortably asleep while a combined loco-regional anaesthesia prevents you to feel any pain.
THE ANAESTHETIST
Anaesthetists are doctors who have had specialist training in anaesthesia, in the treatment of pain, in the care of very ill patients (intensive care), and in emergency care (resuscitation). They will make major decisions with you, although if you are unconscious or very ill, they will make the decisions on your behalf.
Your anaesthetist is responsible for:
- Your wellbeing and safety throughout your surgery and up to 1 or 2 days following your surgery
- Agreeing with you a plan for your anaesthesia
- Giving your anaesthetic
- Planning your post-operative pain control with you
- Managing any transfusion you may need
- Your care in the intensive care unit (if this is necessary)
Our qualified anaesthetists will take care of you as appropriate with the support of anaesthesia technicians.
The anaesthetist and the team
Anaesthetists work closely with surgeons and other staff from operating theatre:
- Operating theatre staff who are trained in anaesthesia, who prepare and maintain equipment, help the anaesthetist and take part in your care;
- Recovery room staff who are specially trained and who will care for you after your surgery until you are ready to go back to the ward;
- Anaesthesia technicians are specialised healthcare professional trained to maintain anaesthesia under the supervision of an anaesthetist. This means they look after the anaesthesia once it is underway. Anaesthesia Technicians are not medically qualified, but they have completed training and assessments for the skills they need. They will always have access to an anaesthetist when they need it.

BEFORE YOU COME INTO HOSPITAL
Here are some things that you can do to prepare yourself for your operation and reduce the likelihood of difficulties with the anaesthetic.
- If you smoke, you should consider giving up for several weeks before the operation. The longer you can give up beforehand, the better. Smoking reduces the amount of oxygen in your blood and increases the risk of breathing problems during and after an operation. If you cannot stop smoking completely, cutting down will help.
- If you are very overweight, many of the risks of having an anaesthetic are increased. Reducing your weight will help. Your General Practitioner (GP) will be able to give you advice about this.
- If you have loose or broken teeth, or crowns that are not secure, you may want to visit your dentist for treatment. The anaesthetist may need to put a tube in your throat to help you breathe, and if your teeth are not secure, they may be damaged.
Health check before your anaesthesia
Before your anaesthesia we need to know about your general health. You will be asked to fill in a questionnaire either at a pre-admission anaesthesia consultation or in the ward after you are admitted to hospital.
You may be asked about:
- Your general health and fitness;
- Any serious illnesses you have had;
- Any problems with previous anaesthetics;
- Whether you know of any family members who have had problems with anaesthetics;
- Any pains in your chest;
- Any shortness of breath;
- Any heartburn;
- Any pains you have which would make lying in one position uncomfortable;
- Any medicines you are taking, including herbal remedies and supplements you may have been prescribed or may have bought;
- Any allergies you have;
- Any loose teeth, caps, crowns or bridges;
- Whether you smoke;
- Whether you drink alcohol;
- Whether you use recreational drugs (drugs that are not prescribed to you or bought over the counter).

The anaesthesia consultation
You will usually meet with your anaesthetist either at a pre-admission anaesthesia consultation or in the ward after you are admitted to hospital. If you need blood tests, an ECG (electro-cardiogram or heart tracing) an X-Ray or other tests, these will be arranged. Some tests can be done on the same day as your consultation, for others you may need to come back another day. This is a good time to ask questions and talk about any worries you may have.
Questions you may like to ask your anaesthetist
- Who will give my anaesthetic?
- Do I have to have a general anaesthetic?
- What type of anaesthesia do you recommend?
- Have you often used this type of anaesthesia?
- What are the risks of this type of anaesthesia?
- Do I have any special risks?
- How will I feel afterwards?
ON THE DAY OF YOUR OPERATION
Nothing to eat or drink – fasting (“Nil by mouth”)
The hospital will give you clear instructions about fasting. It is important to follow these. If there is any food or liquid in your stomach during your anaesthesia, it could come up into the back of your throat and then go into your lungs. This would cause choking, or serious damage to your lungs.
In an emergency (such as needing surgery for badly broken bones), where people have not had time to fast, there are other techniques and drugs that allow anaesthetics to be given safely, which your anaesthetist will explain to you.
Meanwhile, too long fasting before can be detrimental and your anaesthetist may prescribe with energetic drink in the few hours before the anaesthesia. Thank you to comply with this safe prescription.
Your normal medicines
You should continue to take your normal medicines up to and including the day of surgery, unless your anaesthetist or surgeon has asked you not to. However, there are exceptions. For example, if you take drugs to thin your blood (such as warfarin, aspirin or clopidogrel), drugs for diabetes or herbal remedies, you will need specific instructions. If you are not sure at any point, your anaesthetist or surgeon will advise you.
If you feel unwell
If you feel unwell when you are due to come into hospital for your operation, your surgeon and anaesthetist will need to know. Depending on the illness and how urgent the surgery is, your operation may need to be postponed until you are better.
MEETING YOUR ANAESTHETIST
You will have a consultation with your anaesthetist doctor before any surgery to assess which type of anaesthesia is best for you. Your anaesthetist will explain the type of anaesthesia that you will receive. Your doctor may prescribe certain tests prior to surgery (the anaesthesia consultation and requested tests before surgery are not included in the price of your surgical package).
The choice of anaesthesia depends on:
- Your operation
- Your answers to the questions you have been asked
- Your physical condition
- Your preferences and the reasons for them
- Your anaesthetist’s recommendations for you and the reasons for them
- The equipment, staff and other resources available at the FV Hospital

Having talked about the benefits, risks and your preferences, you can then decide together what is best for you.
Nothing will happen to you until you understand and consent to what has been planned for you. You have the right to refuse if you do not want the treatment suggested or if you want more information or more time to decide.
Premedication
Premedication (a “pre-med”) is the name for drugs which are given before some anaesthetics. These days they are not used very often, but if you feel a pre-med would help you, you can ask your anaesthetist about having one.
Most are tablets or liquid that you swallow, but you may need an injection, a suppository or an inhaler.
They can:
- Reduce or relieve anxiety
- Help to prevent sickness after the operation
- Treat any health problems you may have
- Help with pain relief after your operation
They may make you drowsier after the operation. If you want to go home on the same day, this may be delayed.
Needles and local anaesthetic cream
A needle may be used to start giving your anaesthetic. If this worries you, you can ask to have a local anaesthetic cream put on your arm to numb the skin before you leave the ward. The ward nurses will do this.
Blood transfusion
During most operations, you will lose some blood. If necessary, your anaesthetist will make up for this blood loss by giving you other types of fluid into a vein through a drip. If you lose a lot of blood, your anaesthetist will consider a blood transfusion.
If your anaesthetist expects you to need a blood transfusion, he or she will discuss this with you beforehand.
Occasionally, you might need blood unexpectedly. You have the right to refuse a blood transfusion, but you must make this clear to your anaesthetist and your surgeon before the operation.
What blood will I be given?
Your anaesthetist will know your blood type from your records.
Most commonly, you will receive blood from a volunteer (a blood donor). It is supplied by the Blood Transfusion Haematology (BTH) Hospital in Ho Chi Minh City.
Why does the anaesthesiologist postpone some operations?
Occasionally, your anaesthetist might find something about your general health that could increase the risks of your anaesthesia or operation. It might then be better to delay your operation until the problem has been reviewed or treated. The reasons for any delay would always be discussed with you at the time. Your anaesthetist’s main concern is your safety.
Getting ready for ‘theatre’
Here are some of the things that you may be asked to do to get yourself ready for your operation.
Washing and changing
- A bath or shower before your operation will clean your skin and reduce the risk of infection. You must avoid using make-up, body lotions or creams as they prevent heart monitor pads and dressings from sticking to your skin properly.
- You may brush your teeth in this time, but do not swallow the water.
- You will be given a hospital gown to put on.
- Avoid fingernail polish and ask for advice about false nails. These can interfere with oxygen monitoring.
- If you have long hair, tie it back.
Your Valuables while you are in the Operating Theatre
It is preferable not to bring any valuable at the hospital. If you bring any, your nurse will be happy to assist you in securing them in the ward safe. FV Hospital cannot take responsibility for items not locked in the ward safe.
Going to the operating theatre (OT)
If you are to have a general anaesthesia, you will need to remove your glasses, hearing aids and dentures, and leave them in your room. A porter will help you onto a mobile trolley, and your nurse will check your information one last time and escort you to the operating theatre. Two family members are allowed to escort you to the door of the operating theatre but not inside as this is a sterile area.
If you are under sedation or general anaesthetic, an intravenous access (drip) may be inserted into your arm to deliver medications more easily.
The operating theatre
The OT includes a waiting area, anaesthetic rooms, operating rooms and a recovery room. It looks and feels quite different from other hospital departments – more cold and clinical. The operating rooms are brightly lit and have no natural light.
The OT may also be quite cool. As it is important for you to keep warm, a blanket will help if you feel cold.
The staff
Theatre staff normally wear coloured ‘pyjamas’ face masks and paper hats. Because of this, they all look much the same, but you will probably recognise your anaesthetist as you should have met him or her already.
Reception
Theatre staff will ask your name and date of birth and will check them against your identification bracelet and medical records. The staff will also ask you about other details in your medical records as a final safety check that you are having the right operation.
The anaesthetic room
You will then be taken into the anaesthetic room or, sometimes, into the operating room. Several people will be there, including an anaesthetist, who may not be the one that you have seen in consultation, the anaesthesia technician, and OT nurses.
All the checks you have just been through will be repeated once again.
To monitor you during your operation, the anaesthetist will attach you to machines to watch:
- Your heart: sticky patches will be placed on your chest (electrocardiogram or ECG)
- Your blood pressure: a blood-pressure cuff will be placed on your arm
- The oxygen level in your blood: a clip will be placed on your finger (pulse oximeter)
More monitoring may be needed for major operations.
Setting up your cannula
The anaesthetist may need to give you drugs into a vein. A needle will be used to put a thin plastic tube (a ‘cannula’) into a vein in the back of your hand or arm. This is taped down to stop it slipping out. Sometimes, it can take more than one attempt to insert the cannula. You may be able to choose where your cannula is placed.
If you have not been able to drink for many hours before your operation, or you have lost fluids from being sick, you may have become dehydrated. Bags of sterile water with added salt or sugar can be given through a drip into your cannula to keep the right level of fluids in your body. Any blood you may need will also be given through the drip.

LOCAL AND REGIONAL ANAESTHETICS
These anaesthesia are usually given to you while you are awake, either in the anaesthesia room or operating room.
This is so that you can:
- Help your anaesthetist get you into the correct position
- Tell your anaesthetist if the needle causes pain
- Tell your anaesthetist when the anaesthetic is taking effect
The type and place of a local or regional anaesthetic injection will depend on the operation you are having and the pain relief you will need afterwards.
Local anaesthetics
Local anaesthetics are injected close to the area of your operation. They can also be used to numb the skin before anything sharp is inserted, such as a cannula for a drip.
Regional anaesthetics
Spinals or epidurals (the most common regional anaesthetics), are used for operations on the lower half of your body.
Spinal anaesthetics are single injections which take only a few minutes to work and last about two hours. They cannot be topped up to make them work longer.
Epidural anaesthetics can take up to half an hour to work but can be used to relieve pain for hours and sometimes days after your operation. They can be topped up by putting more local anaesthetic into the fine plastic tube.
There are other peripheral nerve blocks that your anaesthetist may be able to offer for specific operations.
Starting a regional anaesthetic
Some local anaesthetic or a light sedation can be given to help the discomfort of the injection for the block.
It can take more than one attempt to get the needle in the right place so that the area is properly numbed. If you find this too painful, you can always ask your anaesthetist to stop, and use other types of anaesthesia.
Your anaesthetist will ask you to keep quite still so he or she can give you your local or regional anaesthetic block. When the needle is inserted, your anaesthetist will ask you if you feel any tingling or shocks.
You may notice a warm tingling feeling as the anaesthetic begins to take effect. It is common to feel as though the part of your body which is anaesthetised does not belong to you.
Your operation will only go ahead when you and your anaesthetist are sure that the area is numb.
Once the local or regional block is working, your anaesthetist will continue with the plan you have agreed.
In the operating room: local or regional anaesthetics
This is often a busy place, with staff bustling to get ready for your surgery and noises echoing around. Music may be playing. You may be moved across from your trolley onto the operating table. Monitoring equipment will be reconnected, bleeps will start indicating your pulse and a cuff will inflate on your arm to take your blood pressure regularly.
A cloth screen is used to shield the operating site, so you will not see the operation unless you want to. Your anaesthetist or anaesthesia technician is always near to you and you can speak to him or her at any time.
After a local or regional anaesthetic
- After surgery you may have problems passing urine. A thin soft tube (catheter) may need to be inserted temporarily into the bladder to drain it. This is more likely after a spinal or epidural anaesthetic, as you will not be able to feel when your bladder is full.
- After a loco-regional anaesthesia involving the lower limb(s) you may experience some weakness even you have recovered normal sensitivity. Please comply with the recommendation while standing up.
- It will take some hours for feeling to return to the area of your body that was numb. This ranges from one hour to about 18 hours depending on the type of anaesthetic injection and is different from one person to another.
During this time, the recovery or ward staff will make sure that the numb area is protected from injury. You can expect to feel tingling as feeling returns, but this soon passes. At this point it is important to let staff know if you are feeling pain.

GENERAL ANAESTHETICS
Starting a general anaesthetic (induction)
Induction usually takes place in the anaesthetic room, although you may go direct to the operating theatre. If you have had premedication to help you relax, you may not remember this later.
There are two ways of starting a general anaesthetic. Either:
- Anaesthetic drugs may be given through the cannula (this is generally used for adults) or
- You can breathe anaesthetic gases and oxygen through a mask.
Induction happens very quickly, and you will become unconscious within a minute or so. People usually describe a light-headed feeling.
If it hurts when anaesthetic drugs are given through your cannula, it is important that you tell your anaesthetist.
Once you are unconscious, your anaesthetist will continue to give drugs into your vein or anaesthetic gases to breathe (or both) to keep you anaesthetised.
In the operating room: general anaesthetics
Your anaesthetist or anaesthesia technician will stay with you and will be constantly aware of your condition, checking the monitors, adjusting the anaesthetic and giving you any fluids or drugs that you need.
These are some of the drugs you may be given during your anaesthetic:
- Anaesthetic drugs to keep you anaesthetised;
- Pain-relieving drugs to keep you pain-free during and after your operation;
- Muscle relaxants to relax or temporarily paralyse the muscles of your body;
- Antibiotics to guard against infection;
- Anti-sickness drugs to stop you feeling sick;
- Other drugs depending on your condition as it changes.
Your anaesthetist will choose a way of making sure that you can breathe easily. He or she may do this by simply tilting your head back and lifting your chin or you may have a tube placed in your airway. Keeping your airway open is essential for your safety.
For some operations, muscle relaxants, which will stop you breathing, are necessary. Your anaesthetist will use a machine (a ventilator) to ‘breathe’ for you.
At the end of the operation, your anaesthetist will stop giving anaesthetic drugs. If muscle relaxants have been used, a drug that reverses their effect will be given. When your anaesthetist is sure that you are recovering normally, you will be taken to the recovery room.
After a general anaesthetic
Most people regain consciousness in the recovery room. Recovery staff will be with you at all times and will continue to monitor your blood pressure, oxygen levels and pulse rate.
- You may receive pain-relieving drugs before you regain consciousness, but if you are in pain, tell the staff so they can give you more.
- Oxygen will be given through a lightweight clear-plastic mask, which covers your mouth and nose. Breathing oxygen keeps up its levels in your blood while the anaesthetic wears off. The staff will remove your mask as soon as these levels are maintained without oxygen.
- If you feel sick, you may be given drugs which will help this.
- Depending on the operation you have had, you may have a urine catheter. This is a thin soft tube put temporarily into the bladder to drain it.
- When you are fully alert, dentures, hearing aids and glasses can be returned to you.
You may shiver after your operation. If you are cold, you will be warmed with a warming blanket..
Intensive Care Unit (ICU)
After some major operations, you may be taken to the ICU. If this is planned, it will be discussed with you beforehand. If you are going to one of these areas, you can ask your surgeon, anaesthetist or ward nurse what to expect.
AFTER YOUR OPERATION

Back to the ward
The recovery staff must be totally satisfied that you have safely recovered from your anaesthetic, and all your observations (such as blood pressure and pulse) are stable before you are taken back to the ward.
The operation will affect how long it will be before you can drink or eat. After minor surgery, this may be as soon as you feel ready. Even after quite major surgery you may feel like sitting up and having something to eat or drink within an hour of regaining consciousness.
What will I feel like afterwards?
How you feel will depend on the type of anaesthetic and operation you have had, how much pain-relieving medicine you need and your general health.
Most people feel fine after their operation.
However, you may suffer from side effects of some sort. You may feel sick, dizzy or shivery, or have general aches and pains. Some people have blurred vision, drowsiness, a sore throat, a headache and breathing difficulties.
You may have fewer of these side effects after a local or regional anaesthetic block. Until the block wears off, you will usually feel fine. When it has worn off, you may need pain-relieving medicines and you may then suffer from their side effects. However, you must take them early as prescribed before the anaesthesia has disappeared. Otherwise you could experience strong pain and more difficulties to control it.
You can find more information about side effects and complications in the index which starts on page [32].
It is important to ask for help:
- When you first get out of bed (although you may feel fine lying in the bed, you may feel faint or sick when you first get up);
If you have had a spinal or epidural, as your legs may still be weak or numb for some hours. They may not regain their full strength for about 12 hours.
First uprising from bed after spine or loco regional anaesthesia of lower limb should be with the support of the nurse.
This will help prevent you from falling over.
PAIN RELIEF
Good pain relief is important. It prevents suffering and it helps you recover more quickly. Your anaesthetist will probably discuss different pain-relief methods with you before your surgery so you can make an informed decision about which you would prefer.
Some people need more pain relief than others. Feeling anxious increases the pain people feel:
- Pain relief can be increased, given more often, or given in different combinations;
- Occasionally, pain is a warning sign that all is not well, so the nursing staff should be told about it. Good pain relief helps prevent complications;
- If you can breathe deeply and cough easily after your operation, you are less likely to develop a chest infection;
- If you can move around freely, you are less likely to get blood clots (Deep-Vein Thrombosis or DVT).
It is much easier to relieve pain if it is dealt with before it gets bad. So, you should ask for help as soon as you feel pain and continue the treatment regularly.
WAYS OF GIVING PAIN RELIEF
Pills, tablets or liquids to swallow
These are used for all types of pain. They take at least 20 minutes to work and should be taken regularly. You need to be able to eat, drink and not feel sick for these drugs to work.
Injections
If needed, these may be given through your cannula into a vein or into your leg or buttock muscle. If they are given in your muscle, they may take 20 minutes or more to work.
Suppositories
These waxy pellets are placed in your back passage (rectum). The pellet dissolves and the drug passes easily into the body. They are useful if you cannot swallow or if you are likely to vomit. They are often used alongside other methods.
Patient-controlled analgesia (PCA)
This is a method using a machine that allows you to control your pain relief yourself. It has a pump which contains an opiate drug (see page [30]). The pump is linked to a handset which has a button. When you press the button, you receive a small dose of the drug painlessly into your cannula.
If you would like more information, ask your ward nurses for a leaflet on PCA.
Local anaesthetics and regional blocks
These types of anaesthesia can be very useful for relieving pain after surgery. More details are in the leaflet ‘Epidurals for pain relief after surgery’.

DRUGS YOU MAY RECEIVE
Opiates
These are the drugs often used for severe pain. They include morphine, diamorphine, codeine and pethidine. They may be given by tablets, injections or patient-controlled analgesia. They may also be added to a spinal or epidural to give longer and better pain relief.
Some people have side effects – the most common include feeling sick, vomiting, itching, constipation, and drowsiness. Larger doses can produce breathing problems and low blood pressure (hypotension). The nursing staff will watch you closely for these. These side effects can be treated with other drugs. Your reaction to opiates will affect you considerably. One in three people finds opiates unpleasant. If they make you very sick, controlling your pain may be more difficult.
Constipation can be a problem. Your nurses and doctors will check on this and treatment can help.
Some other pain relievers
Drugs such as diclofenac or ibuprofen may be given during an anaesthetic, as a suppository or afterwards as tablets. They must be used carefully by people with asthma, kidney disease, heartburn or stomach ulcers. You may also be given paracetamol.
Pain-relief teams
Most hospitals have a team of nurses and anaesthesiologists who specialise in pain relief after surgery.
One of the team may visit you before major surgery to discuss ways to control your pain.
HOW DID IT ALL GO?
For most people, the part that the anaesthesiologist plays in their care is over within an hour or two of day surgery, or a day or two for more major surgery. The anaesthesiologist’s interest in your welfare continues with visits after surgery (postoperative visits) and reports from the pain relief team, when they are needed.
If there have been any problems during the anaesthetic that have affected you or your treatment, you should be told about them. This is not only because you have a right to know, but also so that you can warn anaesthesiologists who may care for you in the future.
What will I feel like later?
You may feel tired or even exhausted after the operation – sometimes for days. This is unlikely to be caused by the anaesthetic. Tiredness may be caused by many things, including:
- Worry before the operation
- Not sleeping properly before or after the operation
- Pain or discomfort before or after the operation
- Loss of blood (causing postoperative anaemia)
- The condition that needed surgery
- Not eating or drinking normally before and after your operation
- The energy used up by the healing process
- Your general health.
BENEFITS AND RISKS OF ANAESTHESIA

Safety in anaesthesia
Anaesthesia has made much of today’s surgery possible, and has brought great benefits. Today, joints can be replaced, organs can be transplanted, and diseased tissue can be removed with a high degree of comfort and safety.
The benefit of anaesthesia is that it will remove pain and sensation. This benefit needs to be weighed against the risks of the anaesthetic procedure and the drugs used. The balance will vary from person to person. It is difficult to separate these risks from those of your operation or procedure and your general health.
The risk to you as an individual will depend on:
- Whether you have any other illness
- Personal factors, such as whether you smoke or are overweight
- Surgery which is complicated, long or done in an emergency.
Everyone varies in the risks they are willing to take. Anaesthesiologists and patients may also hold different views about the importance of risk.
To understand a risk, you must know:
- How likely it is to happen
- How serious it could be
- How it can be treated.
The anaesthesiologist may use many drugs or combinations of drugs. The more complicated the anaesthesia and surgery are, the more chance there is of complications and side effects (listed in the index starting on page [32]).
It is the responsibility of the anaesthesiologist to advise you on what anaesthetic techniques will give you greatest benefit and reduce as far as possible these risks. Making these decisions is difficult but your anaesthesiologist will want to help you, so that you can make the choices that are right for you.
Safety of anaesthetic drugs
Many of the drugs used by anaesthesiologists have been successfully used for a long time. In Vietnam, all drugs must be approved by the Ministry of Health before they can be prescribed.
Anaesthetic patient information leaflets
Like paracetamol or other drugs you buy at the pharmacy, manufacturers provide a patient information leaflet for anaesthetic drugs. This leaflet describes what the drug is for, how it works and what its side effects are. If you want to know more about a drug, ask to see the leaflet.
SIDE EFFECTS AND COMPLICATIONS OF ANAESTHESIA
Anaesthetic risks are thought of in terms of side effects and complications.
Side effects are secondary effects of drugs or treatment. They can often be anticipated but are sometimes unavoidable. Almost all treatments (including drugs) have side effects of some kind. Unpleasant side effects do not usually last long. Some are best left to wear off and others can be treated.
Examples would be a sore throat or sickness after a general anaesthetic.
Complications are unexpected and unwanted events due to a treatment. Examples would be an unexpected allergy to a drug or damage to your teeth caused by difficulty in placing a breathing tube. The risk of something happening to one in 10 people means that, it will not happen to nine out of 10 people.
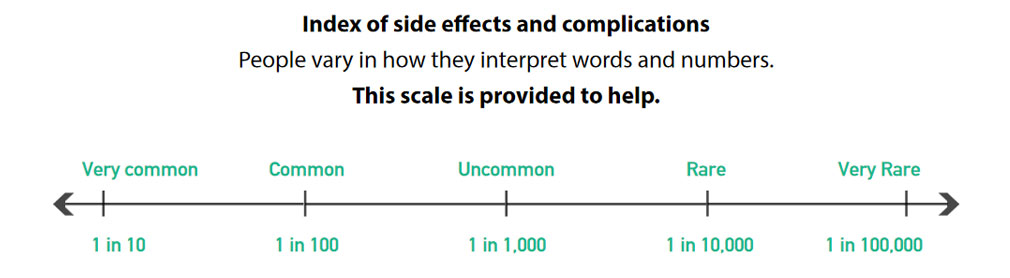
If something is very common, this means that about one in 10 will experience it.
Common means about one in 100.
Uncommon means about one in 1000.
Rare means about one in 10,000.
Very rare means about one in 100,000.
Using this index
This index is divided into three sections which relate to the scale.
There is also a key to show which side effect or complication is relevant to which type of anaesthetic
RA = This may occur with a regional anaesthetic.
GA = This may occur with a general anaesthetic.
Very common and common side effects and complications
Feeling sick and vomiting after surgery GA RA
Some operations, anaesthetics and pain-relieving drugs are more likely to cause sickness (nausea) than others. Sickness can be treated with anti-vomiting drugs (anti-emetics), but it may last from a few hours to several days.
Sore throat GA
If you have had a tube in your airway to help you breathe, it may give you a sore throat. The discomfort or pain lasts from a few hours to days and can be treated with pain-relieving drugs.
Dizziness and feeling faint GA RA
Your anaesthetic may lower your blood pressure and make you feel faint. This may also be caused by dehydration (when you have not been able to drink enough fluids). Fluids or drugs (or both) will be given into your drip to treat this.
Shivering GA RA
You may shiver if you get cold during your operation. Care is taken to keep you warm during your operation and to warm you afterwards. A hot-air blanket may be used. However, shivering can happen even when you are not cold, due to the effects of anaesthetic drugs.
Headache GA RA
There are many causes of headaches, including the anaesthetic, the operation, dehydration and feeling anxious. Most headaches get better within a few hours and can be treated with pain-relieving medicines. Severe headaches can happen after a spinal or epidural anaesthetic (see the leaflet about this listed on the inside front cover of this booklet). If this happens to you, your nurses should ask the anaesthesiologist to come and see you. You may need special treatment to cure your headache.
Itching GA RA
This is a side effect of opiates (such as morphine), but can be caused by an allergy (for example, to drugs, sterilising fluids, stitches or dressings). If you have itchiness, it can be treated with other drugs.
Chest infection GA
A chest infection is more likely to happen to people who smoke, and may lead to breathing difficulties. This is why it is very important to give up smoking for as long as possible before your anaesthetic.
Bladder problems GA RA
After certain types of operation and regional anaesthesia (particularly with a spinal or epidural), men may find it difficult to pass urine, and women tend to leak. To prevent problems, a urinary catheter may be inserted at a suitable time.
Muscle pains GA
These sometimes happen if you have received a drug called suxamethonium. This is a muscle relaxant which is given for emergency surgery when your stomach may not be empty.
Uncommon side effects and complications
Breathing difficulties GA RA
Some pain-relieving drugs can cause slow breathing or drowsiness after the surgery. If muscle relaxants are still having an effect (have not been fully reversed), the breathing muscles may be weak. These effects can treated with other drugs.
Damage to teeth, lips or tongue GA
Minor damage to your lips and tongue is common. Damage to your teeth is uncommon, but may happen as your anaesthesiologist places a breathing tube in your airway. It is more likely if you have weak teeth, a small mouth, a stiff neck or a small jaw.
An existing medical condition getting worse GA RA
Your anaesthesiologist will always make sure that you are as fit as possible before your surgery. However, if you have had a heart attack or stroke, it is possible that it may happen again – as it might even without the surgery. Other conditions such as diabetes or high blood pressure will also need to be closely monitored and treated.
Awareness GA
Awareness is becoming conscious during some part of an operation under general anaesthetic. It happens because you are not receiving enough anaesthetic to keep you unconscious. Monitors are used during the operation to record how much anaesthetic is in your body and how your body is responding to it. These normally allow your anaesthesiologist to judge how much anaesthetic you need to keep you unconscious. If you think you may have been conscious during your operation, your anaesthesiologist should be told about it as soon as possible. He or she will want to know, to help both you and future patients.

Rare or very rare complications
Damage to the eyes GA
Anaesthesiologists take great care to protect your eyes. Your eyelids may be held closed with adhesive tape, which is removed before you wake up. However, sterilising fluids could leak past the tapes, sheets or drapes or you may rub your eye as you wake up after the tapes have been removed. These could cause damage to the surface of your eye, which is usually temporary and responds to drops. Serious and permanent loss of vision can happen, but it is very rare.
Serious allergy to drugs GA RA
Allergic reactions will be noticed and treated very quickly. Very rarely, these reactions lead to death even in healthy people. Your anaesthesiologist will want to know about any allergies in yourself or your family.
Nerve damage GA RA
Nerve damage (paralysis or numbness) can be caused by a needle when performing a regional anaesthetic or can be due to pressure on a nerve during an operation. It varies with the type of anaesthetic you have, but is generally rare or very rare. Most nerve damage is temporary, but in some cases damage is permanent.
Death GA RA
Deaths caused by anaesthesia are very rare. There are probably about five deaths for every million anaesthetics given in the UK.
Equipment failure GA RA
Vital equipment that could fail includes the anaesthetic gas supply or the ventilator. Monitors give an immediate warning of problems, and anaesthesiologists have immediate access to back-up equipment.



