Overview
Osteoporosis is a condition that weakens bones, making them fragile and more likely to break. Often the condition develops slowly over several years, and is only diagnosed when a minor fall or sudden impact causes a bone fracture. Worldwide, osteoporosis causes more than 8.9 million fractures annually, which is equivalent to an osteoporotic fracture every 3 seconds, and typically 1 in 3 women and 1 in 5 men over the age of 50 will suffer from the condition in their lifetime.
In Vietnam alone, according to preliminary data from the Institute of Nutrition, osteoporosis affects 1 in 3 women and 1 in 8 men who are over 50. It is estimated that in the country, 2.5 million people have osteoporosis and over 150,000 suffer from osteoporotic fractures.
Osteoporosis is characterised by low bone mineral density (BMD) and destruction of bone tissue, which both lead to an increased risk of fractures. The bones most commonly affected by osteoporosis include the hip, spine, and wrist. The effects of osteoporosis can be devastating, leading to pain, disability, loss of independence and, in some cases, death. As an example, vertebral fractures are associated with significant long-term disability, pain and kyphosis. low BMD incurs an increased risk of acquiring a fracture, however the most at risk for osteoporosis fractures are postmenopausal women and elderly men.
Commonly, osteoporosis is underdiagnosed and advice on correct medication is often poor. Most people are not aware of their own fracture risk and do not receive appropriate education, screening or management even after they have had a minimal trauma fracture. As a result, one of the largest gaps in it’s treatment is the failure to prevent subsequent fractures.
Key points you should know:
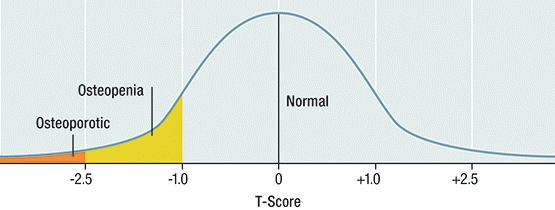
World Health Organisation diagnostic criteria for osteoporosis, osteopenia and normal bone mineral density.
- Refer all patients aged 70 years and over to check their bone mineral density (BMD using Dual-energy Xx-ray absorptiometry (DXA) if they have not done so already.not had one.
- Use a fracture-risk calculator to help high-risk patients understand their own fracture risk and to discuss treatment options.
- Emphasise to patients the importance of taking osteoporosis medication medicines as directed to optimise the effects of their treatment effects.
- ForIn patients suffering from a with minimal trauma fracture, initiate osteoporosis treatment without waiting for a DXA scan.
How to identify high-risk patients:
➢ Recommend a DXA to check a patient’s BMD and screen for osteoporosis in postmenopausal women and men aged over> 50 years in the following cases:
- Previous minimal trauma fracture
- Aged over 70
- Non-modifiable:
- Family history of having fractures
- Modifiable and lifestyle:
- Premature menopause
- Hypogonadism
- Repeated falls
- Immobility/inactivity
- Low body weight or low muscle mass and strength
- Poor balance
- Low protein or calcium intake
- Smoking
- Alcohol – over 2 standard drinks/day
- Vitamin D insufficiency
- Diseases or conditions:
- Rheumatoid arthritis
- Hyperthyroidism
- Hyperparathyroidism
- Chronic kidney/liver disease
- Coeliac disease or malabsorption
- Diabetes mellitus
- Myeloma or MGUS
- Organ transplant or bone marrow transplant
- HIV infection
- Depression
- Anti-androgen therapy
- Medications (large effect):
- Glucocorticoids (over 3 months taking 5 mg or more of prednisolone a day)
- Excess thyroid hormone replacement
- Aromatase inhibitors
- Medications (modest effect)
- SSRIs
- Antipsychotics
- Thiazolidinediones
- Anti-epileptic medications
- PPIs
➢ Refer patients with a height loss of 3 cm or more, kyphosis or new unexplained back pain for a standard spine X-ray.
➢Use “Garvan Fracture Risk Calculator” (GRFC), at https://www.garvan.org.au/promotions/bone-fracture-risk/calculator/, or “Fracture Risk Assessment Tool” (FRAX), at https://www.sheffield.ac.uk/FRAX/ to estimate fracture risk.
How to start osteoporosis medicines:
➢ To treat minimal trauma fractures:
| Minimal trauma fracture is the most important risk factor for a future fracture. An initial fracture increases the risk of a second fracture at least 2-fold for women and 4-fold for men. |
✧ Initiate osteoporosis treatment in patients with a minimal hip or vertebral trauma fracture without waiting for DXA scan result. Note: DXA scan may be useful to provide a baseline BMD.
✧ For other minimal trauma bone fractures at any other site, if BMD T-score is more than> – 1.5, refer patients to a specialist to exclude other causes of fracture and for treatment recommendation.
➢ To treat high-risk patients:
| Corticosteroids suppress bone formation, reduce intestinal calcium absorption and gonadal function, and increase risk of fall due to myopathy.Patients taking more than 7.5 mg oral prednisolone or equivalent during initial 3 – 6 months have significant risk of fracture. The risk continues to increase to a lesser rate as long as corticosteroids are used. |
✧ Initiate osteoporosis treatment in patients who have not had a fracture but:
- Are aAged ≥ 70 or over years old with BMD T-score of ≤ – 2.5 or less, orOR
- Have a hHigh 10-year risk of a potential fracture: hip fracture over > 3%, any fracture over> 20%, or with a T-score ≤ – of 2.5 or less.
➢ To reduce future fracture:
Medications for osteoporosis:
| Class | Recommended for | Avoid in patients | Comments |
| Oral bisphosphonate | ▪Prevention and treatment of postmenopausal osteoporosis and corticosteroid-induced osteoporosis. ▪Treatment of osteoporosis in men. | ▪Who cannot remain upright for at least 30 minutes. ▪With an esophageal or swallowing disorder. ▪Unable or unwilling to follow dosage instructions. ▪With hypocalcaemia. ▪With renal insufficiency (e.g., CrCl under 30 mL/min). | ▪GI side effects: esophagitis, gastritis, dysphagia, abdominal pain, diarrhea, upset stomach and heartburn. ▪May rarely cause severe, disabling musculoskeletal pain. ▪Associated rarely to osteonecrosis of the jaw and atypical femur fracture. ▪Reassess the need for ongoing treatment after 5 years in patients taking bisphosphonate whose T-score is 2.5 or over and have no new fractures. ▪Continue treatment if BMD is under- 2.5, or new fractures have occurred. ▪Reassess patient’s fracture risk annually and restart treatment if there is evidence of bone loss, especially in the hip or further minimal trauma fracture occurs. ▪Doses may be safely held during hospital admissions as drug accumulates in bone and activity continues even after discontinuation. ▪Ensure adequate calcium and vitamin D intake. ▪Osteonecrosis may occur in up to 12% of patients on IV bisphosphonate. ▪IV: Acute flu-like symptoms. Paracetamol may be given to relieve symptoms. |
| Intravenous bisphosphonate | ▪Patient who cannot tolerate oral bisphosphonate due to gastrointestinal issues. ▪Patient unwilling to follow oral bisphosphonate dosage instructions. ▪When there is adherence issue with oral bisphosphonate. ▪Patient with corticosteroid-induced osteoporosis who is not appropriate for oral bisphosphonate. | ▪With hypocalcaemia. ▪With renal impairment (CrCl under 30 mL/min).
| |
| Calcium and vitamin D | ▪Patients taking osteoporosis treatment if their dietary intake of calcium is inadequate. ▪Prevention of fractures in the elderly who are frail or institutionalised.
| ▪With hypercalcaemia. ▪Caution in patients with renal impairment. | ▪Recommended total daily intake of calcium from food and supplements for postmenopausal women and for men 70 and over is 1300 mg3. -Calcium citrate 2.38 g (elemental calcium 500 mg) -Calcium carbonate 1.5 g (elemental calcium 600 mg). -Calcium citrate is better absorbed than calcium carbonate if gastric pH is high (e.g. PPI use) ▪Recommended daily requirement of vitamin D for people 70 and over is 800 international units; this may be from sunlight, diet and/or supplements. |
Patient Education
- Explain to your patients the importance of taking osteoporosis medicine as directed and how to minimise side effects.
- IllustrateExplain to your patients the seriousness and complications of a minimal trauma fracture, especially in at the hip or spine.
- Encourage your patients to exercise in order to improve their musculoskeletal health and reduce their risk of falling and suffering a fracture. Refer them to physiotherapist or exercise physiologist if necessary.
- Explain to your patients that they can prevent osteoporosis, falling and causing fractures by limiting alcohol intake, not smoking, maintaining a healthy weight, having an adequate diet and adhering to safe sunlight exposure.
Reference
- International Osteoporosis Foundation. Facts and Statistics – Osteoporosis incidence and burden. https://www.iofbonehealth.org/facts-statistics#category-14.
- Qaseem A., Forciea M.A., McLean R.M., Denberg T.D. – Treatment of low bone density or osteoporosis to prevent fractures in men and women: a clinical practice guideline update from the American College of Physicians. Ann Intern Med 2017;166:818-39.
- Australian Government, Department of Veteran’s Affairs. Stopping Osteoporotic fractures. June 2018
- Royal Australian College of General Practitioners, Osteoporosis Australia. Osteoporosis risk assessment, diagnosis and management. Available at: https://www.racgp.org.au/download/Documents/Guidelines/Musculoskeletal/osteoporosis-algorithm.pdf
- Johnell O. and Kanis J. A. (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726.



