What is ERCP?
Endoscopic retrograde cholangiopancreatography, or ERCP, is an endoscopic technique that is used to examine and treat problems in the bile and pancreatic ducts, and the gallbladder. The bile ducts are channels that drain bile from the liver and gallbladder; the pancreatic ducts drain the pancreas. Both types of ducts empty into the duodenum, which is the first part of the small intestine.
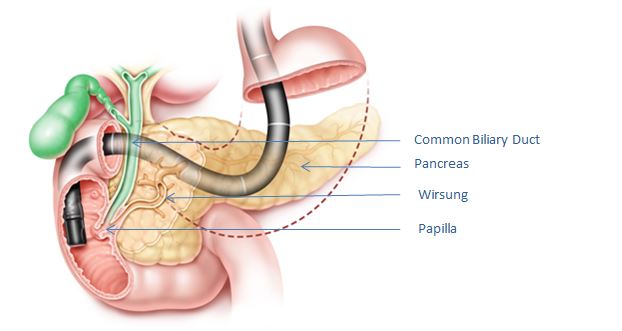
Figure 1. Endoscope in position in the duodenum, facing the papilla; the bile duct is showed in green and the pancreatic duct in brown
Why is ERCP performed?
The most common reason is to find and remove gallstones lodged within the bile duct. Other reasons can include finding causes of persistent pain in the upper abdomen on the right side, looking for causes of acute pancreatitis (acute inflammation of the pancreas) and to relieve obstruction of the bile duct caused by tumours such as pancreas cancer and responsible of jaundice. Often, in many of these situations, an ultrasound of the abdomen or a special kind of Magnetic Resonance Imaging (MRI) study called Magnetic Resonance Cholangio-Pancreatography (MRCP) may be performed to obtain preliminary information that can guide the need for ERCP.
How is ERCP performed?
ERCP is performed by gastroenterologists or surgeons who are specially trained in this technique. An endoscope is a long, flexible tube with a camera and a light at the tip. Since the procedure is performed under sedation or general anaesthesia, you will get a consultation with an anaesthesiologist prior to the procedure.
The endoscope or tube is placed into the mouth and advanced into the oesophagus, stomach, and to the point in the duodenum where the bile duct enters; this is known as the papilla. A plastic catheter (thin tube) is threaded through the scope to come out its tip and then is maneuvered to enter the papilla and the ducts. Contrast dye (radio-opaque material) is then injected into the ducts and X-rays are taken. By examining the ducts in this way, information about blockages, stones, tumours, or irregularities of the ducts can be gathered.
If abnormalities are found, the doctor can perform techniques to repair or improve the condition. For example, if stones are seen, the papilla can be widened or cut open and stones may be removed from the duct with a guidewire. The papilla contains a sphincter muscle that is often cut using cautery (the passage of electric current) during the procedure (sphincterotomy), which allows for better duct drainage. If there is narrowing (stricture) of the bile duct, a short plastic or metal tube called a stent will be placed across the narrowing to drain the bile.
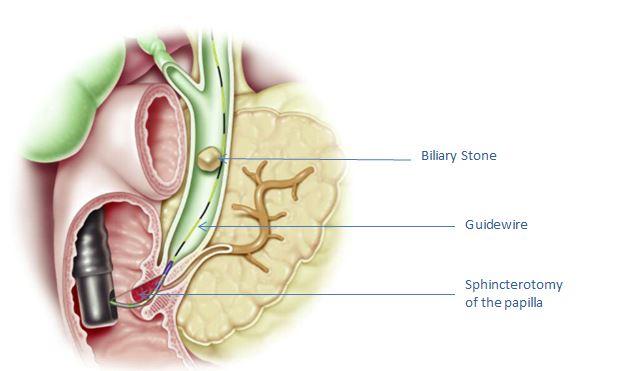
Figure 2. Image showing sphincterotome at papilla, after sphincterotomy has been cut and guidewire in place in the common bile duct, with a large stone in the bile duct.
How do I prepare for ERCP?
You will be required to fast prior to your procedure. The stomach should be empty in order for the stomach to be fully visualised. An empty stomach also decreases the risk of vomiting and aspiration.
You should discuss all current medications with your doctor and the anaesthesiologist, as some may need to be adjusted or temporarily stopped prior to the procedure. This step is especially important if you are taking aspirin, blood thinners (warfarin or heparin), clopidogrel, nonsteroidal anti-inflammatory drugs (NSAIDs), insulin, or other medicines for diabetes. Nonsteroidal anti-inflammatory drugs are common medications used to treat arthritis, pain or inflammation, and include ibuprofen, naproxen, and diclofenac, to name a few. Blood thinning medicines and aspirin or clopidogrel may need to be discontinued several days prior to your procedure. It is also important to discuss any medication allergies, including those to iodine or intravenous contrast dye.
It is important to tell your doctor if you have obstructive sleep apnoea or other lung conditions. If you wear Continuous Positive Airway Pressure (CPAP) at night, you should discuss with your doctor whether you should bring your machine with you on the day of your procedure.
If you have any heart conditions, you should also discuss these with your doctor, as special testing prior to your procedure may be needed.
You will need a family member or friend to accompany you on the day of your procedure in order to transport you home after you have received sedative medications.
What should I expect in the Day Ward?
Upon arriving at the Day Ward (if you are cared with ambulatory procedure), you will answer questions about your medical history and your medications will be reviewed. The ERCP procedure will be thoroughly explained and you will be given a chance to ask any questions that you might have. An intravenous (IV) line will be placed in order to provide IV fluids, sedating medications, and possibly antibiotics. Depending on various factors, you may either undergo conscious sedation (moderate sedation), or general anaesthesia. General anaesthesia is administered by an anaesthesiologist and may require a breathing tube since it is a deeper level of sedation. You will be asked to remove any dentures or eyeglasses prior to being sedated.
You will be brought to the Operating Theatre (OT) room and will be positioned on a special table that allows for X-rays to be taken. You will be asked to lie on your left side, stomach, or back. A small plastic mouthpiece will be placed in your mouth to help protect your teeth and gums. Once sedation is administered, you should expect to be comfortable and asleep or very relaxed. The procedure is generally well-tolerated and most people feel fine afterwards.
Depending on what is seen during the ERCP, a variety of techniques may be performed, including taking biopsies, widening the sphincter (sphincterotomy), removing stones, placing a stent (tube) across any narrowed areas, or other treatments. The length of the procedure varies from 30 minutes to over an hour. Air is introduced through the endoscope so that the endoscopist can see the inside of your stomach and intestine during the examination.
Once the procedure is finished, you will be brought to the recovery room and monitored while the sedative medications wear off. Sometimes patients feel mild abdominal discomfort from the air in the intestines. This is usually relieved by belching or passing gas. A sore throat is a fairly common complaint. It typically resolves in one to two days. You may feel groggy or have difficulty concentrating, so patients are advised to rest for the remainder of the day. You will not be permitted to drive your car for the rest of the day. Depending on your health condition or whether you have a treatment or procedure during the ERCP, you may be admitted to the hospital overnight for observation.
What are the possible complications of ERCP?
While ERCP is generally a safe and well-tolerated procedure, several risks are associated with it. Your doctor should discuss the potential risks with you prior to your procedure.
- Bleeding may occur, particularly if the papilla sphincter is cut. The bleeding is usually minimal and resolves on its own. If it occurs during the procedure, it can be treated with a variety of endoscopic techniques, including placement of hemoclips, injection of epinephrine (which constricts blood vessels), or use of cautery.
- Infection of the bile ducts (cholangitis) can occur, especially if the bile ducts are not draining well. Antibiotics during the procedure and for a few days following ERCP are indicated in certain patients.
- Pancreatitis (inflammation of the pancreas) occurs in 3% to 7% of all patients who undergo ERCP. This would be felt as more severe abdominal pain that does not get better by belching or passing gas. While most post-ERCP pancreatitis is mild, rarely, it can be severe and life-threatening, requiring hospitalisation.
- Perforation (a tear or hole) of the oesophagus, stomach, small bowel, or ducts may occur. While this is a rare complication that may heal on its own, it may be severe, and may even require surgery for repair.
- Aspiration may occur when food from the stomach refluxes into the back of the throat and is inhaled, causing difficulty breathing or pneumoniae. This risk is minimised in patients who have fasted for several hours prior to the procedure.
- Adverse reaction to sedative medicines or anaesthesia.
After going back home, when should I call my doctor?
You should contact your doctor immediately if you experience any of the following symptoms after your ERCP:
- Fever or chills
- Severe abdominal pain
- Vomiting
- Difficulty swallowing
- A crunching sensation underneath the skin
- Severe abdominal bloating with firmness and tenderness
- Bleeding (red, maroon or black stool, or vomiting blood).
- If biopsies were taken during your test, you should follow-up as instructed by your doctor to discuss the results.
GASTRO – ENTEROLOGY & HEPATOLOGY DEPARTMENT
FV Hospital, 2nd Floor, F building
Tel: (028) 54 11 34 66 or (028) 54 11 33 33 – Ext: 1234, 1164



