Neurosurgery is surgery on the brain, spine and peripheral nerves.
A neurosurgeon is a physician who specialises in the diagnosis and surgical treatment of disorders of the central and peripheral nervous system including congenital anomalies, trauma, tumours, vascular disorders, infections of the brain or spine, stroke, or degenerative diseases of the spine
Endovascular Neurosurgery, also called Interventional Neuroradiology, is a subspecialty of neurosurgery.
Endovascular neurosurgeons use catheters and radiology to diagnose and treat various conditions and diseases of the central nervous system. They employ minimally invasive procedures to accomplish a wide variety of treatments, using microcatheters inserted in the groin area and, under X-ray guidance, threaded through the blood vessels leading into the brain or the spine.
Spine Surgery
Back and neck injuries are the most common musculoskeletal problems. In fact, 80% of people will experience back pain at some point in their lives. Pain occurs when the spine, a complex structure of vertebra, disks, the spinal cord, and nerves, is abnormal. When this happens, turning, bending, standing, and lifting become difficult and painful.
The most common problems are herniated disks and stenosis.
- Often, people recover from herniated disks by taking medication and limiting the positions that cause pain. Sometimes, physical therapy also helps. When these treatments don’t work, surgery is an option. During surgery, a neurosurgeon removes the portion of the disk that is protruding. This relieves the pressure on nerves and the resulting pain and discomfort go away
- Often, people with stenosis take medication to relieve pain and reduce inflammation. Steroid injections and physical therapy can also help. For those who do not find relief from these treatments, surgery is an option. The goal of surgery is to relieve pressure in the spinal column by opening up more space inside the spinal canal.
Spondylolisthesis: Common nonsurgical treatment methods include wearing a back brace, doing physical therapy exercises and taking medication to relieve pain. For severe cases of spondylolisthesis may need to have a surgery called a spinal fusion. The surgeon will stabilise the spine by using a bone graft and metal rods. He may insert an internal brace to help support the vertebra while it heals.
Spine congenital conditions (meningocele, tethered spinal cord, dermal sinus)
A meningocele is a birth defect where there is a sac protruding from the spinal column. The sac includes spinal fluid, but does not contain neural tissue. It may be covered with skin or with meninges (the membranes that cover the central nervous system). The sac often is visible from the outside of the back. To close meningoceles at the skull base or top of the spine, our surgeons may use the minimally invasive Endoscopic Endonasal Approach (EEA). This innovative, minimally invasive technique uses the nose and nasal cavities as natural corridors to access hard-to-reach or previously inoperable tumours or lesions. For closing meningoceles lower in the spine, our specialists use minimally invasive spine surgery techniques.
Patients who suffer from advanced degenerative disease of the spine, as well as scoliosis and other kinds of spine deformities, may require complex spinal fusion operations. Such operations use titanium screws to immobilise joints of the spine that are thought to cause pain through mechanisms such as arthritis or spinal instability. In both cases, bones and joints of the spine are moving abnormally.
The goal of a fusion operation is to reduce such patients’ motion-related pain, by locking those bones in place so that the body can convert the abnormally moving joints to solid bone. Only then is the fusion procedure considered successful. Screws and rods must be implanted to prevent motion of the spine while the bony fusion occurs.
Minimally Invasive Spinal Surgery
Compared to open surgical procedures, minimally invasive alternatives offer smaller incisions and reduce post-operative pain, infection risk, and recovery time, and better chance of minimizing damage to normal structures in the surgical area which can help maximize the effectiveness and durability of the surgical treatment
Minimally invasive approaches to treating stenosis and disc disease involve the use of tubes inserted through the skin, through which the entire operation is performed. Minimally invasive spinal surgery techniques for stabilization of the spine can often be used in patients who require spinal fusion due to trauma or advanced degenerative disc and joint disease
Treatment for spine injuries depends on the severity of the injury or injuries. For example, immediate surgery may be necessary to determine the extent of a spinal injury, relieve pressure, or stabilise a fracture to prevent future deterioration and avoid long-term pain or disability
Vertebral compression fractures
Vertebroplasty and kyphoplasty are minimally invasive procedures used to treat vertebral compression fractures of the spine. These painful, wedge-shaped fractures can be caused by osteoporosis and injury. Left untreated, they can lead to a humped spine (kyphosis). By restoring the vertebra height with a balloon and injecting cement into the fractured bone, patients can recover faster and reduce the risk of future fractures.
Brain Surgery
Patients with head trauma may have skull fractures or ruptured brain blood vessels leaking blood onto the surface of the brain, and often have injury to the brain itself caused by these problems. One of the common operations for treatment of these conditions is a craniotomy, which involves surgical removal of a piece of skull to access the brain itself and relieve pressure.
Brain tumours, the growth of abnormal cells in the brain, can be quite complex. Our surgeons have extensive experience with their diagnosis and management and treatment is highly tailored to your individual history and situation. The most appropriate treatment plan will be decided upon through the participation and collaboration of patients, families, oncologists and other doctors involved in your care.
Meningiomas are one of the most common types of brain tumours, and while usually benign, they may be cancerous (malignant). These abnormalities develop in the meninges, the system of membranes that surround your brain and spinal cord.
We also treat tumours that originate in the tissue of the brain itself, called the parenchyma. These include astrocytoma and glioblastoma (both tumours of the support cells of the brain), ependymomas (tumours of the lining of the brain’s fluid-containing ventricles), medulloblastomas (tumours of the cerebellum), and pituitary tumours.
Some pituitary tumours are best managed with medication and some are more responsive to surgery. Minimally invasive techniques using endoscopes to access the pituitary gland avoid making a large incision in the skull (craniotomy), and they reduce pain, infection and complication rates and hospital stay. Working closely with the Department of Otolaryngology (ear, nose and throat surgery), many pituitary tumour surgeries can be performed in this way via the endonasal transphenoidal approach, which allows to avoid the brain and reduce risk of brain injury. In this technique, the neurosurgeon works to access the pituitary gland through the nasal cavity. This technique reduces the risks associated with other, more extensive surgical approaches.
Often, neurosurgical treatment can cure or improve hormonal function enough to enable you to decrease the amount of medication you are taking, or even eliminate the need for medication altogether
Hydrocephalus is a condition commonly referred to as “water on the brain.” The term describes a situation where the ventricles (normal fluid-filled spaces deep in the brain) contain too much fluid or in which the fluid is under excessively high pressure. Hydrocephalus often affects children, and can be caused by inborn conditions, in which a baby’s brain develops abnormally and the proper pathways through which the fluid drains out of the brain are malformed, causing fluid build-up. It can also be caused by brain tumours, intracranial haemorrhage (bleeding in the brain) and other acquired problems.
Hydrocephalus is often treated using a neurosurgical procedure called a ventriculo-peritoneal (VP) shunt, which works like a pipe with an adjustable faucet. A neurosurgeon inserts a catheter directly into brain, through a specially drilled hole, so that the tip ends up inside the enlarged ventricle.
The tube is connected to a valve which controls the flow of fluid out of the brain. The tubing and valve are all located underneath the skin. A magnetic device can be placed over the top of the valve, outside the skin, to permit the surgical staff to adjust the pressure in the valve up or down, like opening or closing a faucet, to drain more or less fluid depending on the patient’s needs.
Cerebrovascular Disorders, Aneurysms, Stroke
We have extensive experience in the diagnosis and management of a broad range of cerebrovascular disorders:
- Aneurysm
- Arterio-venous malformation
- Subarachnoid haemorrhage
- Ischemic stroke and intracranial haemorrhage
- Carotid stenosis
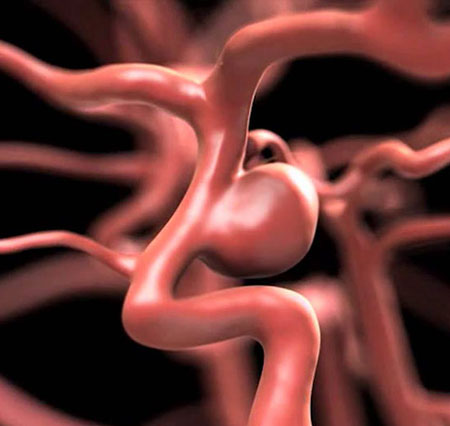
Aneurysms are bulging areas of weakened arteries. Arterio-venous malformations are tangles of thin-walled blood vessels. The danger with both of these conditions is that they can rupture and cause haemorrhage, which may lead to stroke, brain damage or death
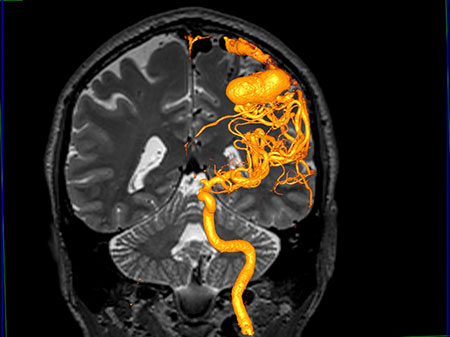
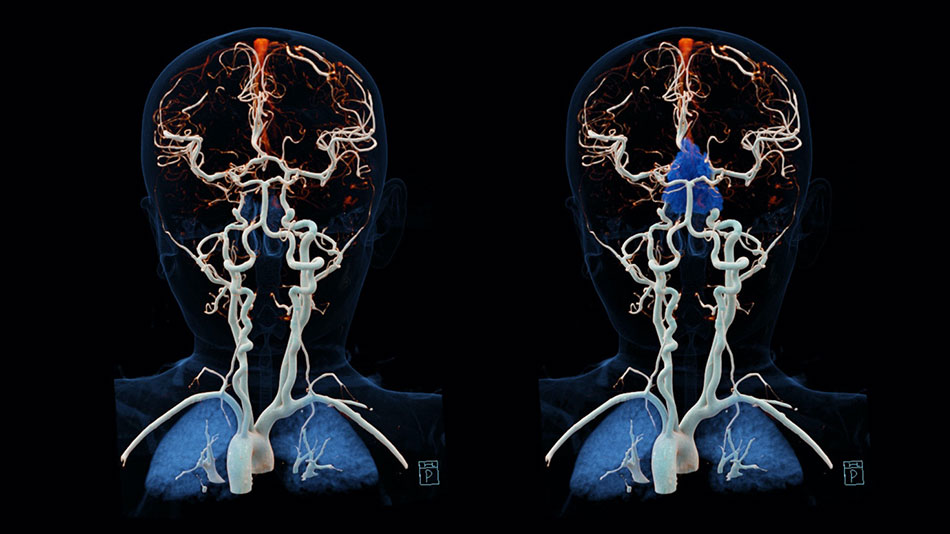
We use the latest diagnostic imaging, such as CT angiogram and catheter-based conventional angiography as well as CT angiography which avoids the risks of catheter techniques, to quickly and accurately diagnose your condition. Our treatments for aneurysms can include open operation (clipping), which involves placing a clamp on the neck of the aneurysm. In addition, we offer non-surgical endovascular treatments
FV Hospital Stroke Unit: patients with acute ischemic stroke can be treated within 45 minutes by thrombolytics
Functional neurosurgery
Trigeminal Neuralgia, Hemifacial Spasm and Pharyngial Neuralgia
One possible cause of both of these conditions is a blood vessel coming in contact with a nerve (the sensory and motor nerve), causing pressure. The trigeminal nerve is affected in trigeminal neuralgia, resulting in pain in the face. The facial nerve is affected in hemifacial spasm, resulting in uncontrollable movement of the facial muscles.
We offer a variety of treatment options, some of which are minimally invasive and some of which involve craniotomy, or open incision. Minimally invasive therapies are often preferred, as they reduce pain, complication and infection rates, and hospital stay. One such alternative is rhizotomy, a needle-based ablative technique that destroys the parts of the trigeminal nerve that causes trigeminal neuralgia.
If traditional open surgery is deemed most appropriate for your condition, we perform a small operation through the skull. This directly reduces the pressure on the trigeminal and facial nerves and can result in long-term pain relief. If a blood vessel is compressing a nerve, the vessel is removed.
Treatment options for chronic pain include using injection treatments, implantable devices and open surgery. We work with the Pain Clinic to coordinate injections of anti-inflammatory medicines and nerve root blocks in the spine as a technique for both diagnosing and treating pain that originates in the neck and back.
In addition, we perform spinal cord and deep brain stimulation for long-term pain that has been resistant to other treatment methods. We also offer microvascular decompression and rhizotomy for trigeminal neuralgia.
A common treatment that is helpful to many patients with certain kinds of pain in the neck and back is pain pump or stimulator implantation. This kind of treatment is appropriate for some patients who continue to suffer from pain after having undergone previous spine operations. We are able to implant specialised devices in your body that deliver medication (pumps) or electrical impulses (spinal stimulators) to the spinal cord via tiny incisions. The medication or electrical stimulation may be able to control your condition or reduce pain.
Peripheral Nerves Surgery
We offer a full range of services to evaluate, diagnose and treat a variety of peripheral nerve conditions, including Carpal Tunnel Syndrome, Ulnar or peroneal nerve compression, brachial plexus injuries, nerve tumours and nerve injuries
Diseases that affect your peripheral nervous system can manifest with pain, sensory disturbance (tingling, burning, inability to know where your body parts are without looking at them, pressure, etc.), motor problems (weakness in moving a muscle or body part) or trouble with the involuntary functions of your body (abnormal sweating, breathing, etc.)
Determination of an appropriate treatment is based on a comprehensive neurological examination that may require additional testing, including electromyogram and nerve conduction studies, imaging studies or nerve biopsy.
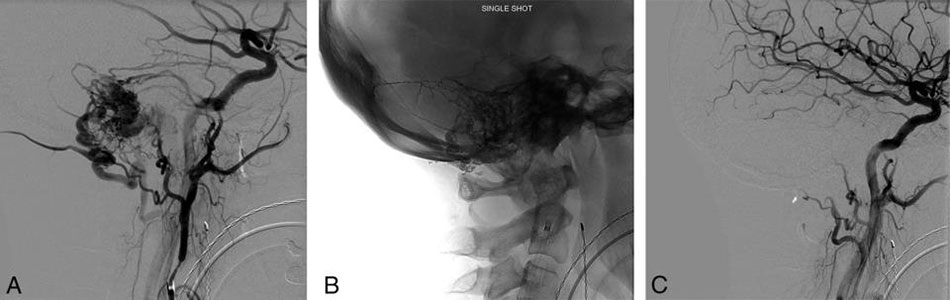
Endovascular Neurosurgery
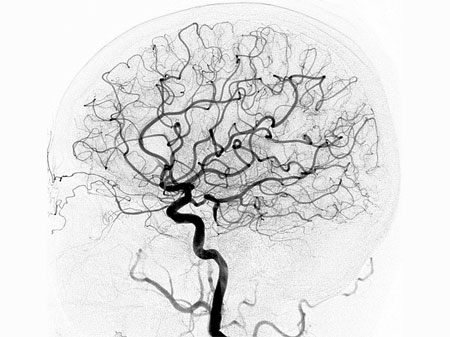
This is a radiology procedure that looks at how blood is flowing in the brain.
Conditions such as cerebral aneurysms, vascular malformations, vascular tumours, strokes and stroke related symptoms can be diagnosed with a cerebral angiogram
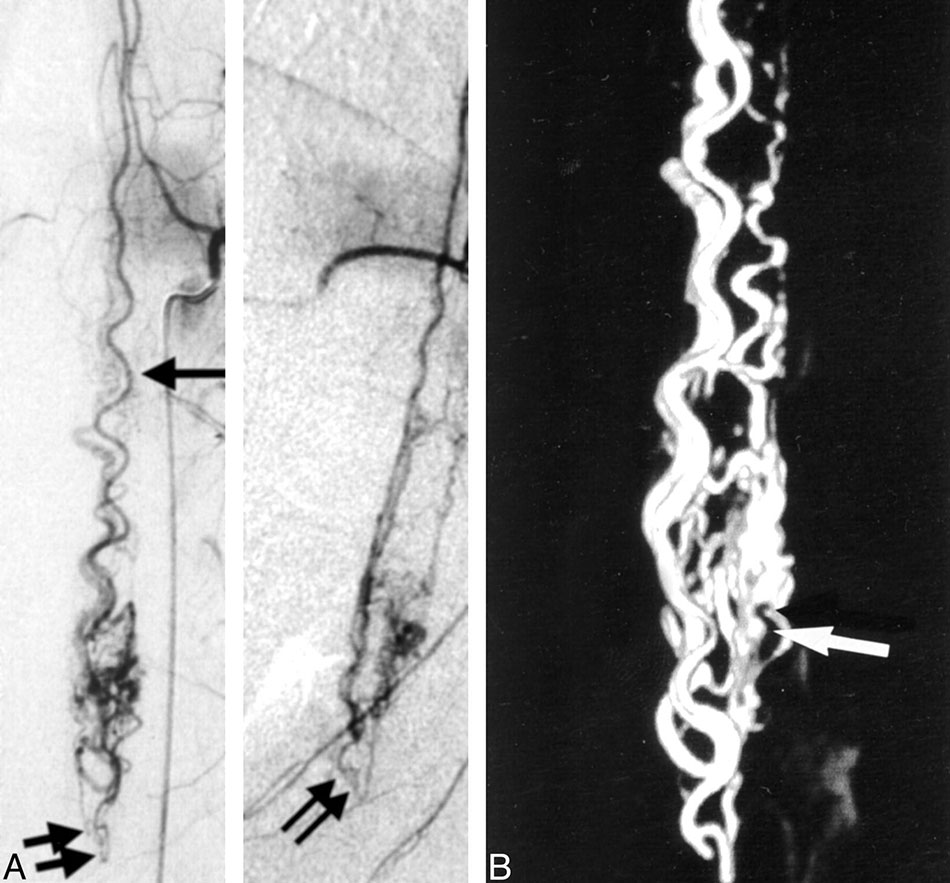
A diagnostic spinal angiography is a medical procedure that offers an extremely precise evaluation of the blood vessels surrounding the spinal cord.
Spinal angiography helps diagnosing medical conditions that involve the arteries and veins of the spinal cord. This typically includes spinal cord vascular malformations, such as dural arteriovenous fistulas (DAVF) and arteriovenous malformations (AVM), but also certain types of spinal cord stroke and disorders involving the spinal cord venous system, such as spinal venous thrombosis
Stroke is the second leading causes of death in the world and is the number one cause of disability. A stroke can be caused by blockage to blood flow in one or more of the arteries supplying the brain (ischemic stroke) or when a blood vessel breaks and starts bleeding into the brain (haemorrhagic stroke).
Conditions such as diabetes, high blood pressure, high cholesterol levels in the blood, and smoking can predispose a person to having a stroke. Symptoms of a stroke can include weakness or numbness in a part of the body, difficulty seeing, or difficulty speaking.
When an ischemic stroke (blockage in blood flow) occurs, it may start either in the brain artery or be caused by a blood clot from the heart, which floats up into a brain artery. When the blockage is complete and lasts long enough, a portion of the brain may die unless the artery is re-opened rapidly.
There are treatments to open the blockages, but they should be performed within a few hours of symptom onset. Giving a clot-busting drug through a vein can treat some strokes. If given early enough after the stroke starts, the drug may open the artery and increase the patient’s chances of making a good recovery. However, sometimes the medication through the vein does not work or the medication cannot be given because the symptoms have been going on too long. In these situations endovascular neurosurgeons can thread a catheter into the brain artery and remove the clot using a number of devices designed to grab the clot and pull it from the circulation

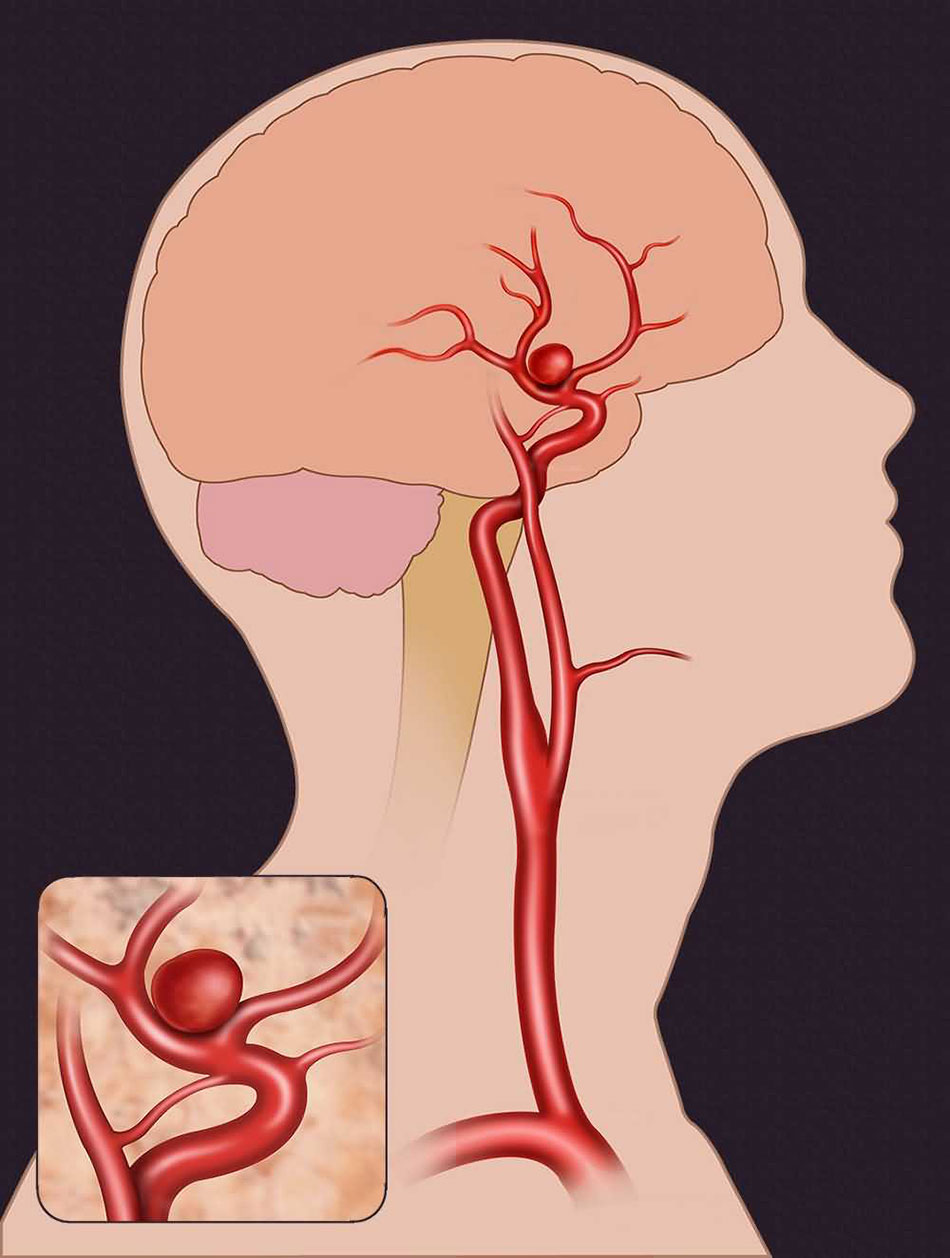
An aneurysm is an abnormal ballooning out of an artery. This occurs when there is a weakening in the wall of the artery and this puts a patient at risk of rupturing or bleeding from the aneurysm. Bleeding from an aneurysm represents a serious medical problem that can cause subarachnoid haemorrhage and is a frequent cause of haemorrhagic stroke.
Aneurysms usually form over time. The average age when a person has symptoms from an aneurysm is usually 40-60 years old, although this can be quite variable. It may be associated with other medical conditions like hypertension and with a history of smoking. About 20% of patients with aneurysms will have multiple (two or more) aneurysms at the same time.
Many patients have no symptoms until the aneurysm ruptures. In some cases, aneurysms can cause headaches or neurologic symptoms before bleeding. Some aneurysms are found prior to breaking or bleeding using CT scanner or MRI. Most people with aneurysms need a cerebral angiography for definitive diagnosis and to determine the best treatment.
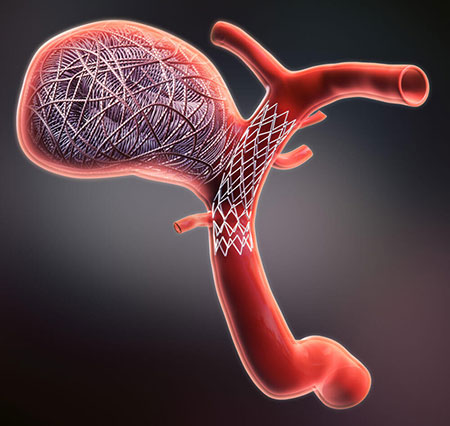
The treatment goal with aneurysms is to close off the aneurysm, thereby eliminating the chance of bleeding. This can be done with a surgical procedure to “clip” the aneurysm or an endovascular procedure to “coil” the aneurysm. Clipping an aneurysm is done by opening the skull and placing a clip over the aneurysm.
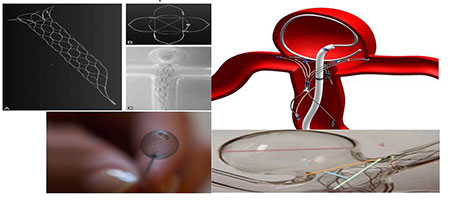
Endovascular treatment of aneurysmsis a technique which greatly benefits patients with serious medical conditions who are unable to sustain the stress of surgery. Platinum coils are guided into the aneurysm via a catheter, creating a clot that effectively closes the aneurysm off from the surrounding circulation, preventing the risk of haemorrhagic stroke in the future.
Larger aneurysms with wider necks or openings are sometimes treated with other endovascular techniques using a balloon to help keep the coils in position inside the aneurysm, or a small stent, which is a small mesh tube that can keep the coils in place.

Atherosclerosis is hardening of the arteries that can result in narrowing (stenosis) or blockage (occlusion) of an artery. This can occur in any artery in the body. Risk factors for the development of atherosclerosis include: high blood pressure, high cholesterol, diabetes, smoking, obesity, and genetic disposition.
When an endovascular neurosurgeon is involved in treating this problem it involves the larger arteries going to the brain (carotid or vertebral arteries) or the arteries inside the head (intracranial arteries).
Atherosclerosis of the carotid arteries often causes transient ischemic attacks (TIAs) because the blood flow may be lowered to the point that a portion of the brain is temporarily not functioning normally. Typical symptoms may include weakness or numbness on one side of the body, inability to speak or understand speech, and changes in vision. If the blood flow is only decreased for a short time a TIA occurs, but if the interruption is sufficiently long a stroke occurs.
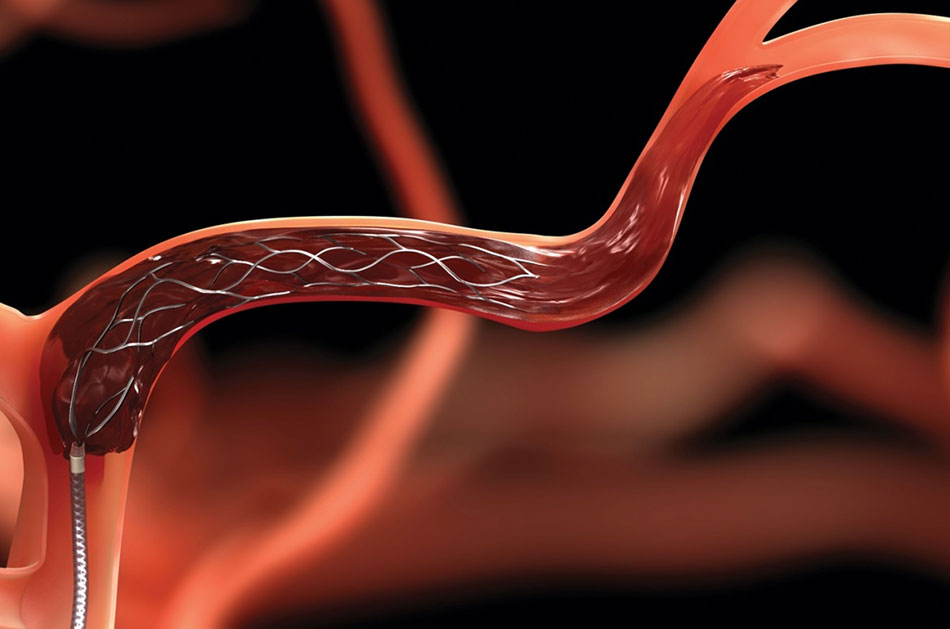
Treatment with medicine may be recommended if the narrowing is not severe. If the narrowing is more severe, surgery or endovascular therapy may be recommended. Surgery involves opening the artery and removing the atherosclerotic plaque that is narrowing it.
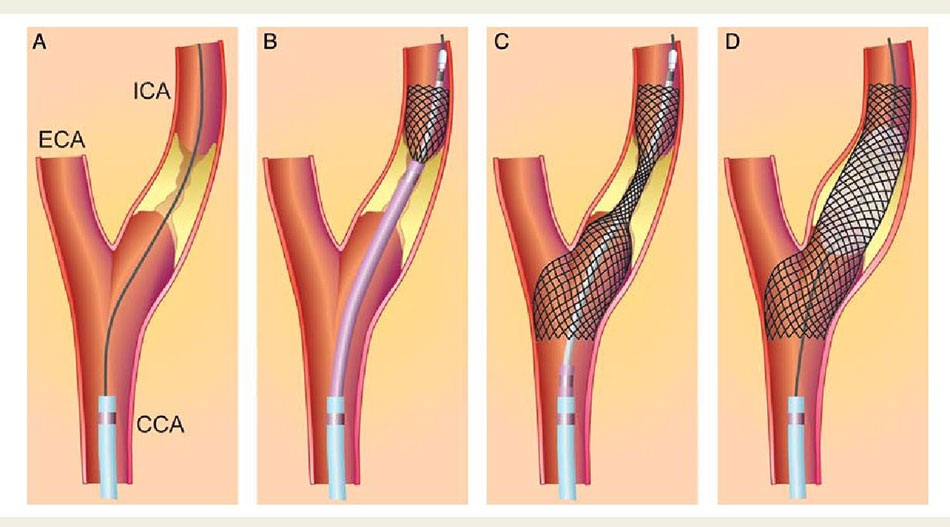
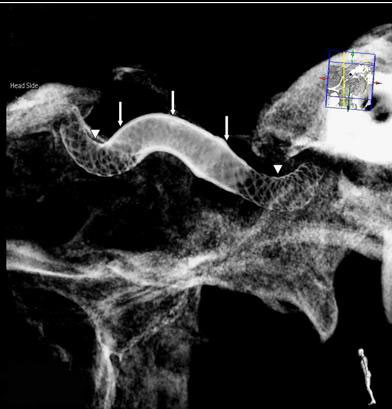
Endovascular therapy involves using a balloon or stent to push open the wall of the artery from within. In the carotid artery, a stent is usually placed to open the narrowing. First, the doctor places an umbrella-like device beyond the narrowed segment to catch any debris that floats off when the stent is put in. Once the stent has been positioned the umbrella is closed and removed from the artery.
Dissection of carotid and vertebral arteries
There are four main arteries that supply blood flow to the brain. Two carotid arteries and two vertebral arteries. The carotid arteries can be felt on each side of the lower neck, immediately below the angle of the jaw. The vertebral arteries are located in the back of the neck near the spine and cannot be felt on physical exam.
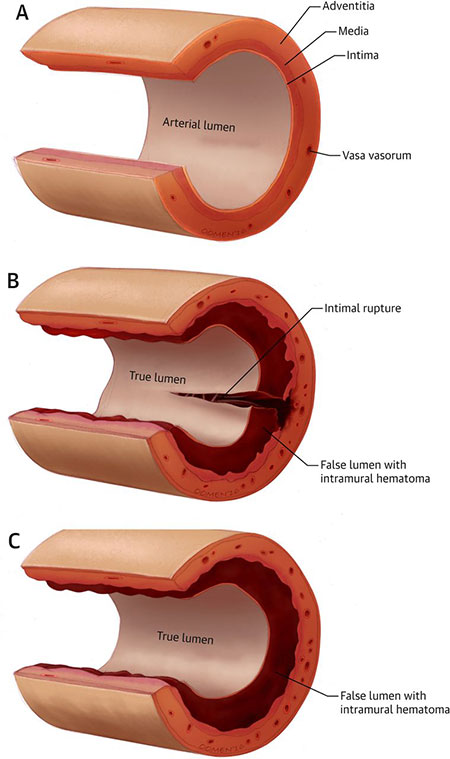
The artery walls are made up of three layers of different types of tissue, each with a specific function. Dissection occurs when a tear in the artery wall allows blood to leak between the layers and separate them.
Sometimes a stroke is the first sign of cervical artery dissection and emergency treatment is required. More commonly, symptoms develop over a period of hours or days, even in patients who have traumatic injuries. Symptoms are general rather than specific and include headache, neck and face pain (especially pain around the eyes), vision disturbances such as double vision or a droopy eyelid, a pulsatile “whooshing” sound in one of the ears, known as pulsatile tinnitus, or a sudden decrease in sense of taste and/or weakness on one side of the body.
Stroke can develop hours, days or even a week after these symptoms begin. This is the most serious risk of cervical artery dissection
Angioplasty (repairing the dissected section of artery with inflation of a special balloon) or placement of a stent (a mesh-like device that holds the artery open) are two endovascular procedures that are used to treat cervical artery dissections. They frequently are used together to provide the longest-lasting treatment

Carotid-cavernous fistulae are a specific kind of dural fistula that involves the carotid artery (or its branches) and a large vein (cavernous sinus) behind the eye. These fistulae can occur because of trauma, if there is an aneurysm in the carotid that breaks and causes the communication, or they can happen spontaneously without a definite reason.
Symptoms can include eye pain, swelling and redness of the eye, double vision or loss of vision if untreated. These fistulae are often treated by an endovascular approach, putting a catheter in the artery or vein, and using material to block up the connection between the artery and vein. This material can include balloons, coils, and liquid glue.


Arteriovenous malformations (AVM)
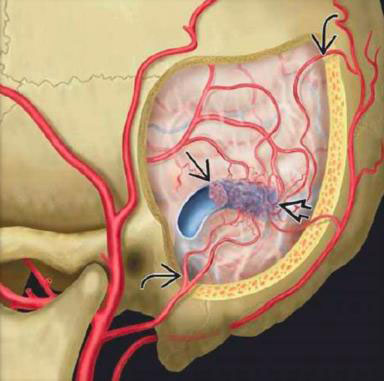
Arteriovenous malformations are abnormal collections of blood vessels, where arteries are directly connected to veins. Normally blood flows through arteries under high pressure to supply all of the organs of the body including the brain. From the arteries, blood passes through thin-walled capillaries to supply oxygen and nutrients to the tissue of the brain and then enters the veins under low pressure to be carried back to the heart and lungs.
In an AVM, the blood flows from the arteries directly to the veins. There is no capillary bed. Without a capillary bed, the AVM blood vessels have an increase in flow and blood pressure. Over the years this causes them to dilate and become thin-walled, and more likely to break and bleed.
An AVM can cause headache, weakness, numbness, visual problems, or seizures. Patients often first show symptoms when there is a bleed or rupture from one of the blood vessels making up the AVM.
An AVM is often diagnosed with a CT scan or MRI. A patient usually requires an angiography to then fully identify the anatomy of the AVM and make decisions about treatment.
AVMs may be treated using three different treatment methods. These methods are embolization, surgery and radiation therapy or radiosurgery.
Endovascular treatment of AVMsis available at FV Hospital. One innovative form of treatment involves use of a “super glue” substance introduced via a tiny catheter to reduce the size of the AVM and facilitate further microsurgical or radiation treatment. In some cases, it is possible to completely block off and cure the AVM with endovascular treatment alone.


Dural arteriovenous fistulae (AVF) are blood vessels that represent abnormal connections between arteries and veins that are found in the covering of the brain. This covering is known as the dura, hence the name. There is a direct connection between the arteries and the vein without any vessels between.
These fistulae or abnormal connections usually develop over time and can occur after trauma, infection or thrombosis (clotting-off) of veins in the dura. The fistula may cause abnormal noises in the head due to the high flow of blood. They can also cause headaches or result in bleeding into the brain.
The treatment is similar to those available for AVMs and can include embolization, surgery, and in some cases radiosurgery. Embolization is often used as the primary therapy to treat this problem. Embolization is performed by placing a tiny catheter directly into the AVF. Embolic material is then injected into the blood vessel to block them up. The embolic material leaves the catheter as liquid and solidifies within the AVF blood vessel to block it up. Sometimes coils are also used to block up the AVF.
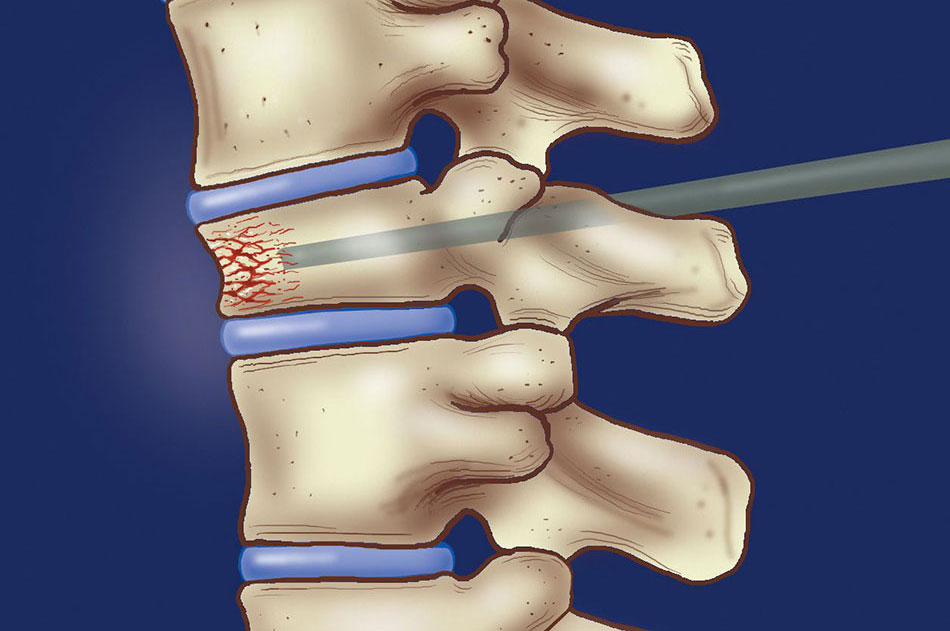
The spinal column is made up of thirty-one individual bones called vertebrae. When they become weakened either because of disease or secondary to medications, they can break or collapse. This is called a compression fracture. Sometime a tumour grows in the bone and weakens it and can cause a compression fracture.
Since it is not possible to immobilize the vertebra completely, patients can have severe pain with movement or secondary to nerve compression. In the past, the only way that this problem was treated was with bed rest, narcotic medication, and in some cases back bracing.
Now, endovascular neurosurgeons are able to offer a procedure called percutaneous vertebroplasty. This procedure is done under radiological guidance, so safe needle placement can be monitored closely. The neurosurgeon inserts a small needle directly into the vertebral body that is compressed. Once needle placement has been confirmed, Polymethylmethacrylate, a type of bone cement, is injected. This essentially strengthens the bone from within.
This procedure has been very effective in decreasing pain, decreasing medication usage, and increasing patient mobility, and is also very safe.

Vascular tumours that come to the attention of the endovascular neurosurgeons may be inside the skull (intracranial) or outside, in the head and neck region (extracranial), or in the spinal column.
Endovascular embolization of vascular tumours is often done as a pre-operative procedure. The goal of this embolization is to reduce the amount of blood loss that is experienced at the time of surgery and also to make the removal of the tumour easier and potentially more complete.
The types of tumours that may respond favourably to this technique include:
- Haemangioma
- Meningioma
- Haemangioblastoma
- Paraganglioma
- Malignant bone tumour
- Juvenile nasal angiofibroma
- Schwannoma
The embolization is performed by placing a catheter directly into the blood supply of the tumour. Embolic material is then injected through the catheter to close off the blood vessels supplying the tumour. This embolic material can include particles, such as polyvinyl alcohol, as well liquid embolic material, which leaves the catheter as a liquid and solidifies within the blood vessel.
The Vein of Galen malformation is a congenital communication between arteries and veins. In this case, the communication specifically occurs between a set of deep arteries in the brain called the choroidal arteries and a deep midline vein, the Vein of Galen.
Often a Vein of Galen malformation will present with symptoms in early infancy or in childhood. In early infancy, these symptoms can include congestive heart failure. Symptoms may occur somewhat later in childhood and the child can manifest enlargement of the head (macrocrania) or a neurocognitive development delay.
In general, the treatment of this disease depends upon the size of the Vein of Galen malformation and the symptoms experienced by the patient. Endovascular therapy is often a mainstay of treatment. This usually involves embolization, often with liquid embolic material (glue) or platinum coils to help occlude (fill) the abnormal communications between the arteries and the veins.
Imaging

CT Scanner
- FV is equipped with the new high-performance Somatom Definition Drive from Siemens with the unique Dual Source technology which boosts accuracy and precision
- A CT scan of the brain may be performed to assess the brain for tumours and other lesions, injuries, intracranial bleeding, structural anomalies such as hydrocephalus, infections, brain function or other conditions, particularly when another type of examination such as X-rays or physical examination are not conclusive.
- A CT scan of the brain may also be used to evaluate the effects of treatment on brain tumours and to detect clots in the brain that may be responsible for strokes. Another use of brain CT is to provide guidance for brain surgery or biopsies of brain tissue.
- A CT scan of the spine may be performed to assess the spine for a herniated disk, tumours and other lesions, the extent of injuries, structural anomalies such as spina bifida (a type of congenital defect of the spine), blood vessel malformations, or other conditions, particularly when another type of examination, such as X-rays or physical examination, is not conclusive. CT of the spine may also be used to evaluate the effects of treatment of the spine, such as surgery or other therapy.
MRI
- FV Hospital is equipped with the Optima MR360 1.5Tesla from GE
- MRI is a diagnostic test that produces three-dimensional images of body structures using magnetic fields and computer technology. The images result from different water concentrations of the various tissues. MRI is an important tool in planning surgery, radiation therapy, treatment for stroke or other interventions for brain and spine disorders.
- MRI may be used for the following diagnostic purposes:
- Detecting brain and spinal cord tumours
- Diagnosing nervous system disorders such as multiple sclerosis
- Identifying diseases of the blood vessels including stroke
- Diagnosing pituitary diseases
- Detecting spinal stenosis and herniated discs

Cath-lab
- FV is equipped with the Allura Xper FD20 from Philips
- The cath-lab allows for neuroradiology investigations such as cerebral angiography and for specialised treatment such as carotid artery angioplasty/stenting
Operating Theatre
- Operating microscope Carl Zeiss
- Mayfield skull clamps
- Microsurgery instruments
- C-arm
- Sonopet Ultrasonic Aspirator from Stryker for microsurgical removal of brain tumours
No results found...