Table of contents
- What is diabetes?
- What are the most common types of diabetes?
- How often should you screen for diabetes?
- How is diabetes diagnosed?
- What are the goal and normal value for diabetes?
- What are the common signs and symptoms of diabetes?
- What are some serious complications of uncontrolled diabetes?
- How do you manage episodes of overly low blood sugar?
- How do you manage episodes of overly high blood sugar?
- What are some medications used to treat diabetes?
- How do you adjust your lifestyle when you have diabetes?
What is diabetes?

After eating, most food is turned into glucose, the body’s main source of energy. As sugar enters the bloodstream, the amount of sugar in the blood rises, and that rise will signal the pancreas to send the hormone “insulin” into the bloodstream. Insulin is produced by the pancreas, an organ that lies behind the stomach. It helps sugar to enter the cells to be immediately used for energy or stored for later use.
When you have diabetes, the food you eat cannot be used for energy because your body is not making enough of insulin or the insulin you have is not working properly. Therefore, sugar stays trapped in the bloodstream, raising the amount of sugar in your blood to abnormally high levels.
Diabetes can, and must, be treated. High blood sugar levels can cause serious health problems. Talk to your doctor or health clinic for more information.
What are the most common types of diabetes?
Type 1 diabetes
About 1 in 10 people with diabetes have Type 1. It usually occurs in children, adolescents or young adults. The body makes little or no insulin; therefore, sugar stays in the bloodstream, and you don’t have enough energy to keep you healthy. People with type 1 diabetes will need insulin shots daily.
Type 2 diabetes
Type 2 diabetes is more common in adults, but the number of children and young people with type 2 diabetes is growing. With type 2 diabetes, your body makes some insulin, but not enough. Or, the insulin your body makes does not work right.
Eating healthy foods, in the right amounts, and being physically active can help people lowering their blood sugar
How often should you screen for diabetes?

The American Diabetes Association (ADA) recommends that adults age 45 and older get screened for type 2 diabetes every three years by their health care provider.
You may need earlier or more frequent diabetes screening if you are overweight AND have one or more of the following risk factors:
- Family history of diabetes (a parent or sibling with the disease)
- African-American, Hispanic-American, Native-American, Asian-American, or Pacific Islander ancestry
- History of blood glucose problems
- History of gestational diabetes (diabetes during pregnancy) or a baby weighing over nine pounds (or 4 kilograms)
- High blood pressure
- Cholesterol problems
- Polycystic ovary syndrome (PCOS)
- History of vascular disease
How is diabetes diagnosed?
Fasting blood sugar (blood sample is taken after 8 to 12 hours without food) of 126 mg/dL (7 mmol/L) or greater
OR random blood sugar of 200 mg/dL (11.1 mmol/L) or greater in patient with classic symptoms of high blood sugar
OR 2-hour blood sugar of 200 mg/dL (11.1 mmol/L) or greater during an oral glucose tolerance test (OGTT)
OR HbA1c level is 6.5% or greater
Note: In the absence of unequivocal high blood sugar, result should be confirmed by repeated testing
What are the goal and normal value for diabetes?
A normal fasting blood sugar range for a person who does not have diabetes is less than 100 mg/dL (5.5 mmol/L).
A target blood sugar range is a range that people with diabetes should try to achieve. The ADA recommends the following targets for most non-pregnant adults with diabetes.
| Level for people without diabetes | ADA goal for people with diabetes | |
| Blood sugar before meals | LESS than 100 mg/dL (5.5 mmol/L) | 70-130 mg/dL (3.9-7.2 mmol/L) |
| Blood sugar after meals | LESS than 110 mg/dL (6.1 mmol/L) | LESS than 180 mg/dL (10 mmol/L) |
| HbA1C | 4-6% | LESS than 7% in most cases |
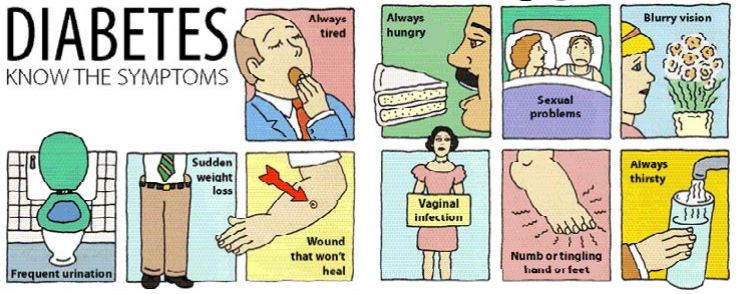
What are the common signs and symptoms of diabetes?
- Increased thirst
- Frequent urination
- Fatigue
- Blurred vision
- Frequent infections
- Increased hunger
- Unexplained weight loss
- Non-healing wounds
- Tingling or numbness of the hands and feet
- Sexual dysfunction
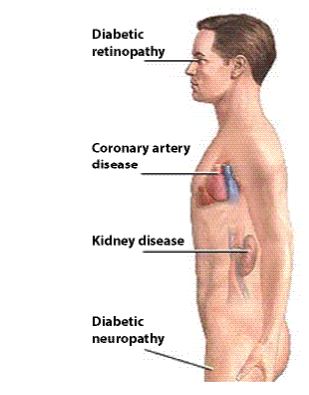
What are some serious complications of uncontrolled diabetes?
Retinopathy: damage to the retina in the back of the eye
- Prevention is KEY
- Have an annual eye exam
- Maintain good blood sugar and blood pressure control
- Call your eye doctor immediately if you have sudden eyesight changes such as black spot, flashing lights, or cobwebs in your eye
Nephropathy: damages to small blood vessels in the kidneys that cause them to leak excess protein into the urine and decrease their ability to filter
- Prevention included testing for microalbumin or protein in the urine annually
- Maintain good sugar level and blood pressure under control
- Take blood pressure pills to protect kidney
Neuropathy: damages to the nerves that cause them to not work properly
- Signs and symptoms: numbness, tingling, or pain in your hands and feet, erectile dysfunction.
- Goal is to maintain good blood sugar level in control
- Prescription medications that treat neuropathy include gabapentin or pregabalin
- Erectile dysfunction medicines are available. Talk to your doctor about that
- Foot care:
- Examine your feet everyday and look for breaks in skin, blisters, calluses, and red or infected areas
- Apply lotion on top and bottom of feet, but not between toes
- Trim toe nails straight across
- Wear socks all the time, even at home to protect your feet
- Get your feet examined by a specialist at least once a year
Heart and blood vessels diseases: including heart attack and stroke
- Maintain good blood sugar and blood pressure level
- Get a lipid profile test at least once a year
- Stop smoking
- Exercise regularly
- Eat a balanced diet
- Take daily aspirin as recommended by your doctor
How do you manage episodes of overly low blood sugar?
Sign/Symptoms:
- Weakness
- Shakiness
- Sweating
- Fast heartbeat
- Irritability/anxiety
- Blurred vision
- Hunger
- Headache
Management: Rule of 15
- When symptoms occur, make sure that you check your blood sugar level. If it comes out less than 70 mg/dL (3.9 mmol/L)
- Eat or drink 15 grams of fast acting sugar: 4 glucose tablets, half a cup of juice or regular soda, 5 to 6 hard candies.
- Check blood sugar level again after 15 minutes. If it’s still low, eat another 15 grams of fast sugar.
- If the blood sugar level is still low after 15 minutes, call the emergency.
Note: If the person is unconscious or unable to swallow, use glucagon emergency kit where available, otherwise call the emergency immediately.
How do you manage episodes of overly high blood sugar?
Sign/Symptoms:
- Extreme thirst
- Frequent urination
- Drowsiness
- Dry skin
- Slow-healing wound
- Blurred vision
- Hunger
Management:
- When symptoms occur, make sure that you check your blood sugar level more frequently (e.g., every couple of hours).
- Drink fluids – at least 8 ounces (240 mL) every hour.
- Maintain adequate carbohydrate intake.
- Continue prescribed medications.
- Call your doctor or go to the emergency right away:
- If your blood sugar is more than 240 mg/dL (13 mmol/L) twice in a row (during 2-6 hours) OR if your blood sugar is more than 240 mg/dL (13 mmol/L) and your urine ketones tests show moderate or large amounts of ketones (for type 1 diabetes).
- If you have severe fever, confusion, shortness of breath or fruity odor on breath.
- If you have severe nausea, vomiting or diarrhea for over 4-6 hours.
- If you are severely dehydrated.
DO NOT WAIT TO GO TO THE EMERGENCY!
What are some medications used to treat diabetes?
Note: NOT all the medications listed below are available in Vietnam and some medications also exist in combination with another drug. Check with your doctor or pharmacist for more information.
Oral medications
| Brand name | Generic name | When to take | How it works | Side Effects |
| Glucophage® Glucophage XR® | Metformin | With meals | Keep the liver from releasing excess glucose (sugar) Tell your doctor if you have liver or kidney problem Hold medication if having procedure where dye is injected into your body
| Nausea, diarrhea, bad taste
|
| Diamicron MR® | Gliclazide | With meals | Enhance pancreas to produce more insulin | Low blood sugar Weight gain |
| Amaryl® | Glimepiride | 15 minutes before meals | ||
| Glucotrol® Glucotrol XL® | Glipizide | 30 minutes before meal | ||
| Diabeta® | Glyburide | 30 minutes before meal | ||
| Prandin® | Repaglinide | 5 – 30 minutes before meals | ||
| Starlix® | Nateglinide | 5 – 30 minutes before meals | ||
| Pioglite® Actos® | Pioglitazone | With or without meals | Help the body make better use of insulin. May take up to 6 weeks to work. Need liver function test before starting therapy and periodically thereafter.
| Possible swelling of the feet and hands, weight gain, liver dysfunction
|
| Avandia® | Rosiglitazone | With or without meals | ||
| Glucobay® | Acarbose | With first bite of food in each main meal | Slow down sugar absorption in the intestine | Nausea, diarrhea, flatulence |
| Miglitol | With first bite of food in each main meal
| |||
| Invokana® | Canagliflozin | Before first meal of the day | Increase sugar release through urine Use caution in patients with kidney disease, low blood pressure, or high potassium level | Yeast infections, urinary tract infections, increased urination |
| Farxiga® | Dapagliflozin | Before first meal of the day | ||
| Januvia® | Sitagliptin | With or without meals | Slow breakdown of gut hormone which increases insulin production and release, and decreases glucagon secretion | Headache, upper respiratory symptoms |
| Onglyza® | Saxaliptin | With or without meals | ||
| Galvus® | Vildagliptin | With or without meals | ||
| Trajenta® | Linagliptin | With or without meals | ||
| Nesina® | Alogliptin | With or without meals | ||
| Cycloset® | Bromocriptine | Take with food in the morning | Increase dopamine receptor activity in brain | Nausea, headache, low blood pressure, constipation |
Injectable medications
Non-insulin products
| Brand name | Generic name | When to take | How it works | Side Effects |
| Byetta® Bydureon® | Exenatide | Up to 60 minutes before breakfast and evening meal | Stimulate insulin secretion when blood sugar is rising Slow glucose release in liver Give a feeling of fullness | Nausea, weight loss
|
| Victoza® | Liraglutide | With or without meals | ||
| SymlinPen® | Pramlintide | Before meals with at least 30 grams of carbohydrates | Help insulin lower blood sugar after meals | Nausea, low blood sugar |
Insulin products
| Insulin | Onset | Peak | Duration | Note |
| Rapid-acting insulin | ||||
| Lispro (Humalog®) Aspart (Novorapid®) Glulisine (Apidra®) | <15 minutes | 0.5 -3 hours | 3 – 5 hours | If mixing with NPH, rapid-acting insulin should be drawn first. Mixture need to be used immediately |
| Short-acting insulin | ||||
| Regular (Actrapid®) | 0.5 – 1 hour | 2 -4 hours | 4-8 hours | |
| Intermediate-acting insulin | ||||
| NPH (Insulatard®) | 2-4 hours | 4-10 hours | 10-12 hours | Should look uniformly cloudy or milky |
| Long-acting insulin | ||||
| Glargine (Lantus®) | 4-6 hours | Same action throughout the day | 20-24 hours | Do not mix with other insulin |
| Levemir (Detemir®) | 2-3 hours | 6-8 hours | Dose dependent: from 6 to 20 hours
| |
| Premixed insulin | ||||
| Mixtard® 30 | 0.5 hour | 2-12 hours | 18-24 hours | 30% regular + 70% NPH |
| Novomix® 30 | 10-20 minutes | 1-4 hour | 18-24 hours | 30% aspart + 70% aspart protamine |
| Humalog Mix 75/25 | 15-30 minutes | 1.6-5 hours | 14-24 hours | 25% lispro + 75% lispro protamine |
| Humalog Mix 50/50 | 15-30 minutes | 0.8-4.8 hours | 14-24 hours | 50% lispro + 50% lispro protamine |
General information on insulin:
- Insulin is synthetically made today in laboratories. It is referred to as human insulin.
- Always store UNopened pen or vial in the refrigerator (2-8oC). Do NOT freeze.
- Most insulin last around 28 days after opening at room temperature (~25oC). Insulin detemir lasts 42 days after opening. Check with your pharmacist for more information.
- Never inject cold insulin. Wait until pen warms up to room temperature
- Always check the expiration date of the insulin and make sure the insulin has no foreign particles in it.
- Always wash hands with soap and water before an injection
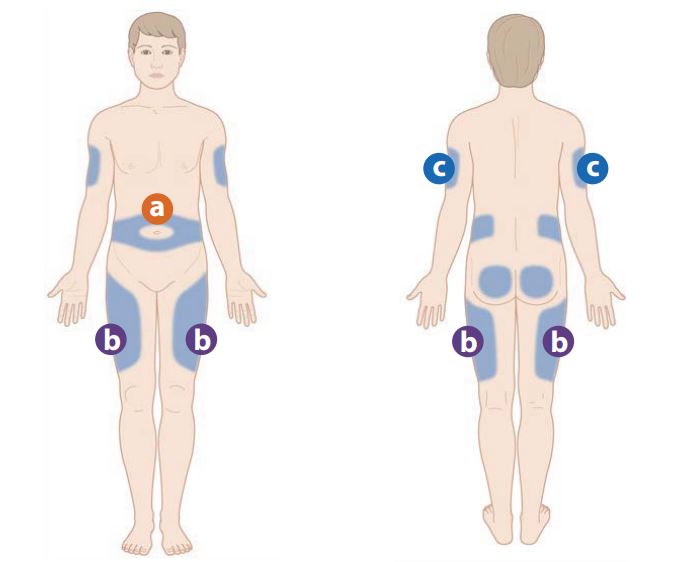
- Injection Sites: insulin is injected into fatty tissues in the abdomen (1), on both sides of the thighs (2), upper hip, or the back of the upper arms (3). Rotate sites every few days for best absorption and avoid fat tissue built-up.
- Always use a new needle for each injection and never share needles or pen with another person.
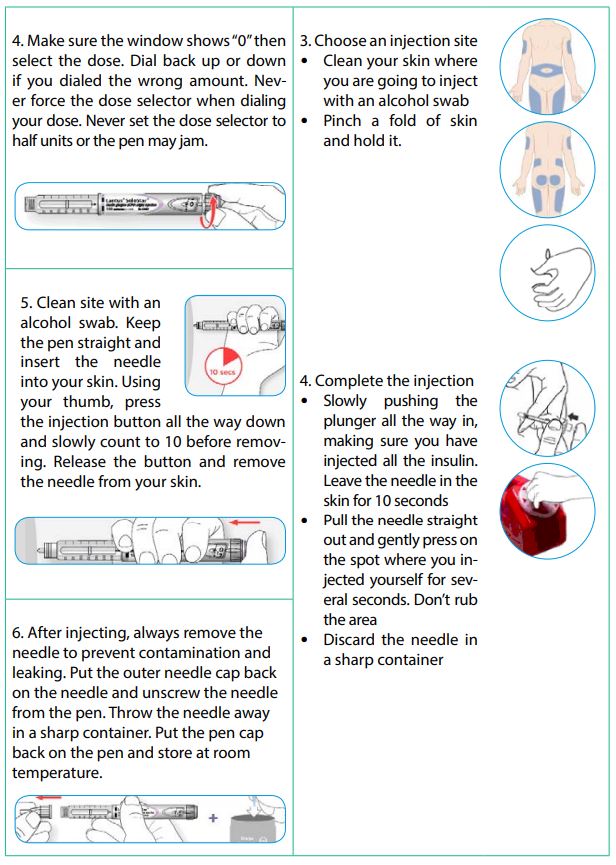
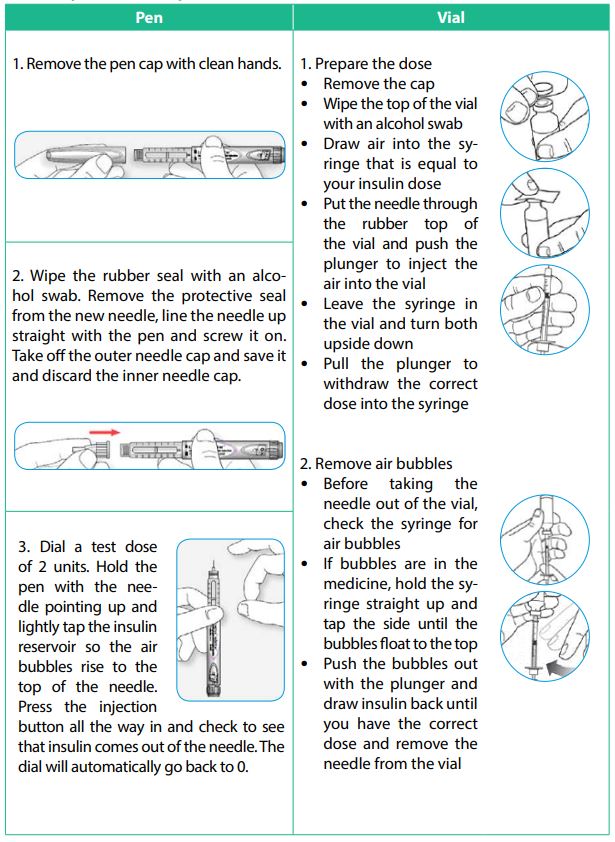
Insulin injection technique
How do you adjust your lifestyle when you have diabetes?
STOP SMOKING!

EXERCISE!
ADA recommends at least 150 minutes of aerobic exercise each week. You can break this up into 30-minute sessions 5 days a week. Exercising every day is ideal.
Examples of aerobic exercises are jogging, brisk walking, biking, rowing, and swimming.
Consult your doctor if you want to add resistance training to your workout. Lifting weights builds muscle, and help control your blood sugar and your weight.
A combination of aerobic exercise and resistance training provides the greatest benefits for people with diabetes.

LOSE WEIGHT!

Maintaining a healthy weight helps your body make better use of insulin. The combination of weight loss and exercise is the best way to improve blood sugar control.
Healthy eating means that you are not eating too little or too much calories. The most important thing is balancing what to eat.
Every person has an individualized balance.
The sources of calories that human body absorbs are carbohydrates, protein, and fat. Make sure you eat foods from each of these food groups.
Most of the carbohydrates you eat enter your blood within a couple of hours. Protein and fat are slower to digest and do not affect blood sugar as quickly as carbohydrates do.
Carbohydrates
- Carbohydrates are the main source of energy of the body. They also affect blood sugar the most.
- The body needs at least 130 gram of carbohydrate per day for basic function.
- Sources of carbohydrates:
- Bread, pancakes, muffin, hamburger bun, cereals, pasta, rice
- Starchy vegetables: corn, pea, potato, pumpkin
- Dairy: milk, yogurt
- Sweets: jam and jelly, syrup, honey, cookies, ice cream, cake.
Fat
- The main goal is to reduce saturated fat, trans fat, and increase fiber and unsaturated fat.
- The body needs around 40 – 70 grams of fat in a day
- Saturated fats raise total cholesterol and low-density lipoprotein (LDL – bad cholesterol), which increase the risks for cardiovascular diseases
- Sources: cream, cheese, butter, lard, and fatty meats
- Unsaturated fats mainly come from plants and include both monounsaturated and polyunsaturated fats. Both are high in total fat and have as many calories as saturated fats, but they are healthier options compared to saturated or trans fats.
- Sources: avocado, most nuts, peanut butter, vegetable oil
- Your dietician may also suggest omega-3 fatty acids for you.
- Sources: fish such as salmon or mackerel, fish oil, soybeans, flax seed (ground)
Protein
- Protein provides nutrients for building cells, tissue, bones and muscles.
- The body needs around 60 – 90 grams of protein in a day.
- Sources: meat, seafood, eggs, nuts, seeds, beans, tofu
- Meat can have a lot of fat. Buy lean meats or remove fat from meat before cooking.
TIPS ON HEALTHY EATING:
- ADA states that alcohol can be part of your diabetes plan only if your blood sugar is in good control. The general guidelines are 1-2 servings with a meal only.
- Spread carbohydrate through out the day. Eat some carbohydrates at each meal, but don’t eat too much at one time.
- Protein, fat, and fiber don’t raise your blood sugar as rapidly as carbohydrates. When you eat these, your blood sugar will rise more slowly.
- Limit saturated fat. Eat lean meat or grilled chicken or fish instead.
- Consult a dietician to learn more about counting carbohydrates, reading food labels and individualizing your meal plan.
- Choose my plate is a useful tool to help you building a healthy plate at meal times.
- Make at least half your grains whole grains and eat a variety of whole grains
- Focus on fruits and eat plenty of fruits of all different colors
- Go lean with proteins – choose fish, poultry, beans, and nuts
- The more vegetables and the greater the variety, the better



