Table of contents
Atrial Fibrillation (AF) is a common and serious disturbance of the electrical system of the heart. It is one of a number of conditions commonly referred to as ‘arrhythmias’ where the heart beats with an abnormal rhythm. If not recognised and correctly treated, AF can result in
significant problems, including stroke and heart failure.
HOW IS THE HEART NORMALLY WORKING?
The heart is a highly efficient pump with 4 chambers. The 2 small upper chambers are called the right and left atria. The 2 larger, lower chambers are called the right and left ventricles.
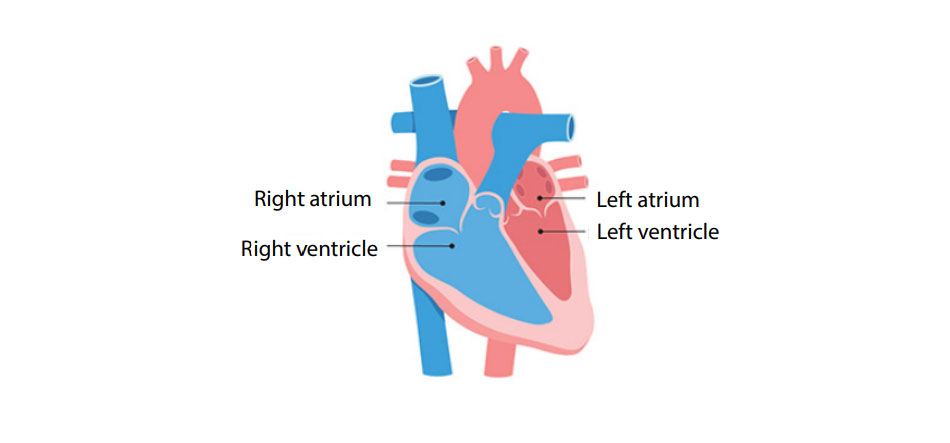
The 2 chambers on the right side of the heart receive oxygen-poor blood (blue) from the body and pump this blood to the lungs, where it receives oxygen. The oxygen-rich blood (red) returns to the left side of the heart, and the 2 left chambers pump this oxygenated blood to the rest of the body. In a normal heart, the atria contract (squeeze) first, pushing blood into the ventricles. The ventricles then contract; the right ventricle pumping the blood out to the lungs and the left ventricle pumping blood to the rest of the body. This process repeats at a regular rate, usually around 60 to 90 times every minute.
WHAT IS ATRIAL FIBRILLATION?
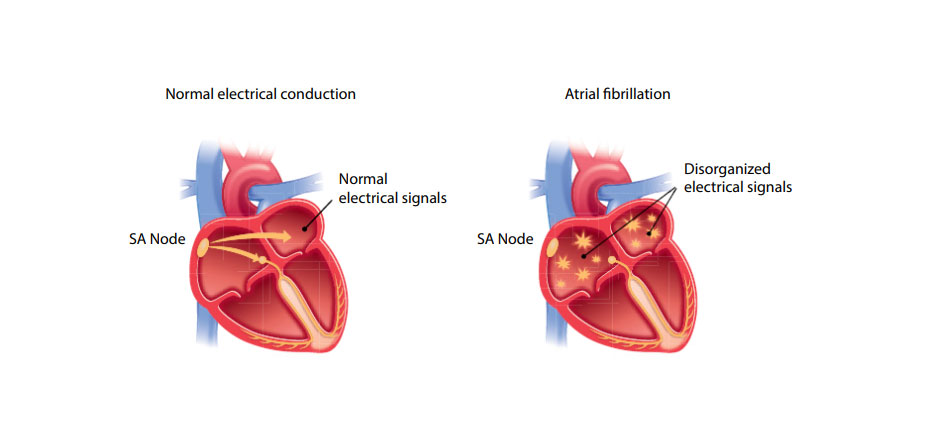
The heart pumping is controlled by your heart’s electrical system.
The contraction of the atria is set off by tiny electrical signals that come from the heart’s natural ‘pacemaker’; a small area of the heart called the sinus node (SA node), located in the top of the right atrium. These signals travel rapidly throughout the atria to ensure that all the muscle fibres contract at the same time, pushing blood into the ventricles. These same electrical signals are passed on to the ventricles and cause the ventricles to contract a short time later, after they have been filled with blood from the atria. This normal heart rhythm is known as ‘sinus rhythm’, because it is controlled by the sinus node.
In AF, there are abnormal electrical impulses in the atria, ‘waves’ of uncontrolled electrical signals travel through the atria, rather than the normal, highly regulated signals from the sinus node. These signals cause the muscle fibres in the atria to contract out of time with each other, and the atria ‘quiver’ (or, in medical terms, ‘fibrillate’). Some of this abnormal electrical activity is passed on to the ventricles, causing a rapid and irregular heartbeat.
WHAT ARE THE SYMPTOMS OF AF?
If you have AF, you may experience palpitations, you become aware of your heartbeat and you may feel irregular heartbeats. Some people may notice that they have an irregular pulse.
AF may also cause general feelings of fatigue, weakness, difficulty exercising, discomfort or dizziness, chest pain. These symptoms occur as the heart is not pumping efficiently. This may even result in fainting or collapse.
Some people with AF may not notice any symptoms, however, it is still important to treat the condition, as it can lead to other problems.
WHAT CAUSES AF?
The most common causes of AF are long-term high blood pressure, coronary heart disease (reduced blood flow to the heart caused by clogging of the coronary arteries) or valvular heart disease (problems with the valves of the heart that normally keep blood flowing in the right direction). Another less common, but treatable, cause is hyperthyroidism (an overactive thyroid gland).
AF can also be associated with chest trauma and/or surgery, caffeine intake and drinking too much alcohol. Certain types of medicine, as well as some diseases such as pneumonia, can ‘trigger’ AF, but sometimes there is no apparent cause – it just happens.
Some people experience AF as a one-off episode; in others, it may come and go (‘paroxysmal’ AF) or persist (‘permanent’ or ‘chronic’ AF).
WHY IS IT IMPORTANT TO RECOGNISE AND TREAT AF?
AF can cause a number of symptoms, as described above, and may indicate an underlying heart or blood vessel disease.
Stroke
One of the most important problems associated with AF is that it may lead to the development of a blood clot inside the atria. This can happen when the atria are not beating properly. In this situation, the blood does not flow normally through the heart, allowing blood to ‘pool’, leading to an increased risk of a clot forming. A portion or portions of this clot (‘emboli’) can break off and be carried from the heart through the bloodstream into smaller and smaller blood vessels, until they get stuck, potentially blocking the blood supply to important organs. If the blockage occurs in a blood vessel supplying the brain, it can cause a stroke. This can damage or destroy brain cells which will affect your body functions.
Without medicines or treatment, the risk of stroke among people aged over 65 years with AF is about one in 20 per year, which is 5 to 6 times higher than those of similar age.
Long-term damage to the heart
Your heart can be damaged over time by having an uncontrolled heart rate for weeks or months like in AF. It reduces the heart’s ability to pump as well as it needs to. This can lead to long-term complications, such as heart failure and other heart conditions.
HOW IS AF DIAGNOSED?
If AF is suspected, a number of tests, including an electrocardiogram (ECG) and echocardiography (ultrasound of the heart) are usually done to confirm the diagnosis and look for any underlying cause (e.g. diseased heart valves) before treatment options are considered.
A 24-hour ECG recording (Holter Monitor) can be used when the standard ECG doesn’t pick up an irregular heartbeat. You wear a small recording machine for 24 hours or longer, usually around your waist. The machine record your ECG continuously during the day and overnight.
Please refer to our brochure ‘Holter monitor’.
WHAT TREATMENTS ARE AVAILABLE?
The best treatment for AF depends on a number of factors, including:
- The severity of symptoms
- The cause (if known) and duration of AF
- The person’s overall risk of stroke and other problems caused by emboli
- The risks of a particular therapy for that person.
Most people with AF will need to take medicine to prevent blood clots from forming. In addition, treatments may be needed to prevent the heart from beating too fast or to restore and maintain a normal heart rhythm.
In some people, such as those with infrequent AF, long-term medicine may be all that is required to treat their condition. In people with chronic AF, cardioversion techniques may be used to restore a normal heart rhythm. If these approaches can’t be used or are unsuccessful, ablation procedures may be considered.
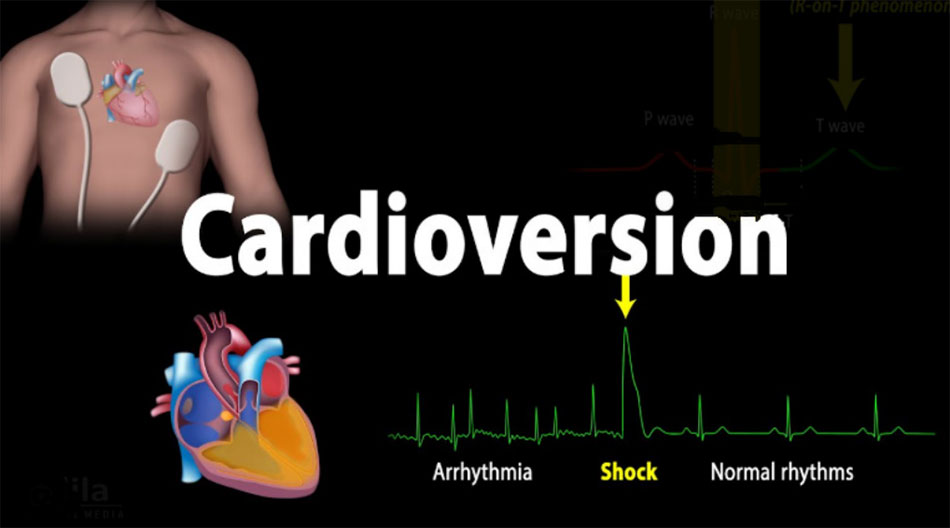
Cardioversion – restoring normal rhythm
For people with a prolonged or particularly serious episode of AF, cardioversion may be used to return the heart to a normal rhythm. After cardioversion, long-term medicines are often prescribed to prevent AF recurring.
- Electrical cardioversion
In this procedure, the heart is given an electrical shock (while under an anaesthetic) to help restore a normal rhythm. Electrical cardioversion is very safe; the main risk is the procedure could dislodge a blood clot that may have already formed in an atria. This risk is small and reduced further by checking for existing blood clots with a test called a ‘trans-oesophageal’ echocardiogram (which takes ultrasound images of the heart from inside the oesophagus) and by giving the person blood-thinning medicines before and after the procedure. Electrical cardioversion only takes a few minutes. The procedure is usually done as a day case, so you will not need to stay in hospital overnight.
- Pharmacological cardioversion
Some medicines (such as flecainide, and amiodarone) can be used to return the abnormal electrical rhythm of the heart to normal. This is known as ‘pharmacological cardioversion’. These medicines may be given as tablets or as an injection, and may also need to be taken regularly in the longer term to maintain heart rhythm.
Slowing the heart rate and maintaining normal rhythm
Some medicines, such as digoxin, beta-blockers and some (but not all) calcium channel blockers, help to slow the heart rate by increasing the time taken for the ventricles to fill with blood before they contract and pump the blood to other parts of the body. Others (including sotalol, flecainide and amiodarone) are known as ‘antiarrhythmic agents’, and work by normalising and maintaining the electrical rhythm of the heart.
Thinning the blood
Most people with AF will be prescribed medicine to thin the blood to prevent clotting. This will decrease your risk of stroke or other problems caused by emboli. The decision to prescribe one of these blood thinning medicines will be based on a balance between reducing the risk of blood clots and emboli forming and the likelihood of excessive bleeding in an individual patient, which will be assessed by your doctor.
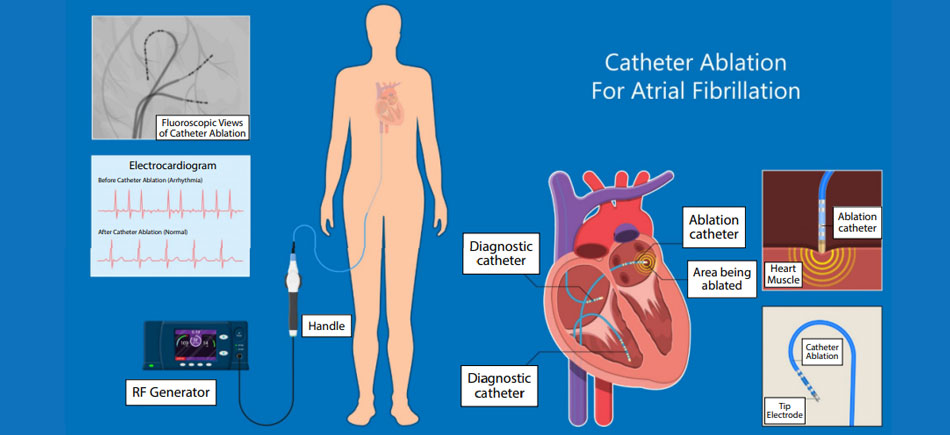
Catheter ablation
This ablation is a non-surgical procedure. A long, thin tube (or ‘catheter’) is inserted into a blood vessel in your groin and moved into your heart. The electrode at the tip of the catheter senses your heart’s electrical signals and takes electrical measurements. Your doctor tests your heart and then ‘ablates’ sections of the muscle tissue using the catheter. Catheter ablation can be done using:
- Intense cold (‘cryoablation’)
- High-frequency energy (‘radiofrequency ablation’)
- High-voltage electrical pulses (‘Pulse field ablation’).
LIFESTYLE MANAGEMENT
In most people, AF can be well controlled, and they continue to lead a relatively normal and healthy lifestyle. However, as AF is often associated with other forms of cardiovascular disease, people with the condition should act to minimise common risk factors for heart disease.
Avoiding smoking, avoiding or significantly reducing alcohol, enjoying healthy eating, being physically active, controlling blood pressure and achieving and maintaining a healthy body weight are important ways to minimise the risk of cardiovascular disease. People with diabetes should make sure that their diabetes is well controlled.
Go for regular check-ups. They will help you maintain your quality of life.



