Corneal Transplantation has advanced to a stage where long term success rates and visual outcomes can be excellent, even in the most severe cases, and several different forms of Corneal Transplantation are now available to suit the disease condition.
If you have received, or will be receiving a cornea transplant, or are a relative or friend of a patient, this document provides you with important information about corneal transplant surgery at FV Hospital, and what is required for corneal transplant patients to ensure maximum success before, during and after surgery.
The aim of this document is to introduce you to some basic facts about the cornea, and corneal transplant surgery, and help you understand the nature of your eye condition, and how to take care of yourself after the corneal transplant has been performed. Understanding the need for proper aftercare and support after surgery is essential in the long term success of the transplant, and for you to continue to enjoy good vision.
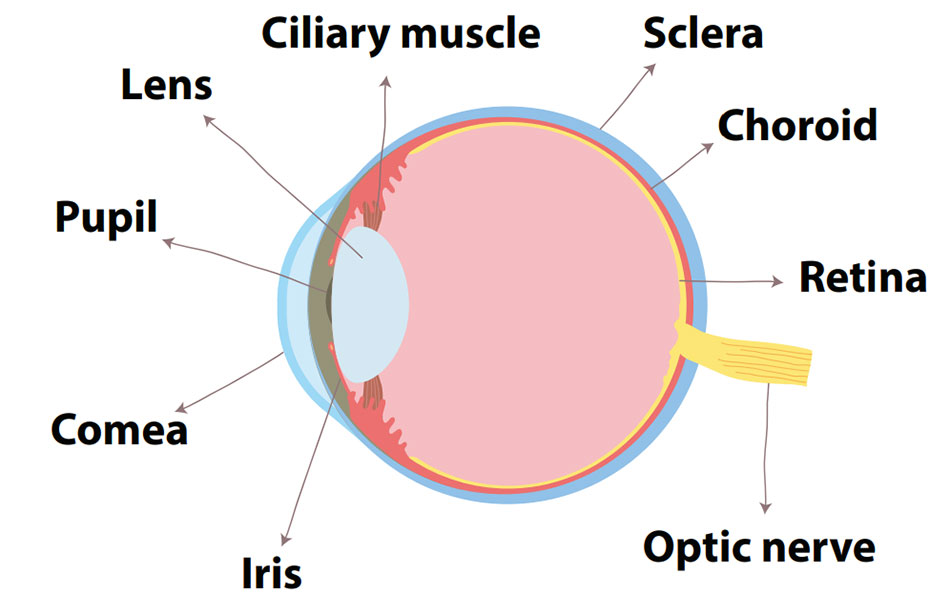
THE CORNEA
The cornea is the clear transparent window at the front of the eye, allowing light to focus and enter the eye. If the cornea is damaged or distorted by injuries or infection, or becomes cloudy due to various corneal diseases, vision may be significantly reduced, or lost.
The Cornea has several layers consisting of different tissue layers – some corneal diseases affect only inner or outer layers, which other corneal diseases may affect all the layers of the cornea.
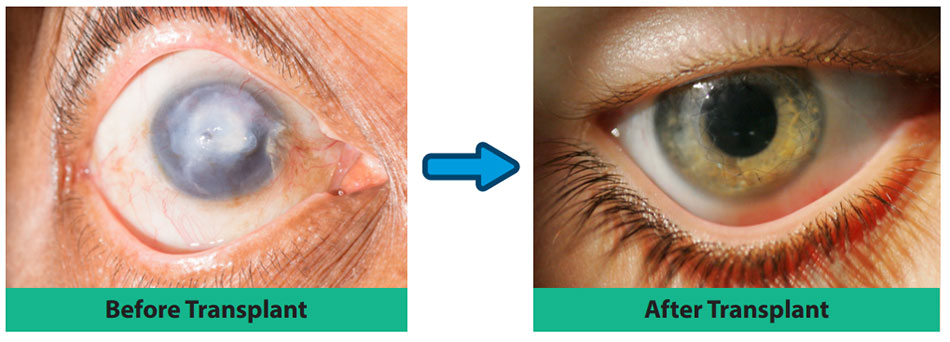
Corneal Transplantation (or Corneal Graft) is a surgical eye operation, in which the diseased layers of the cornea are replaced by healthy donor corneal tissue donated by another individual when he or she passes away. The replacement of the cloudy cornea, with a clear and healthy new cornea, restores vision to the corneal transplant patient.
TYPES OF CORNEAL TRANSPLANTATION
The Cornea consists of several layers, and in many patients, not all the layers are diseased or damaged. In the past, corneal surgeons only performed one main procedure – the Penetrating Keratoplasty (PK) operation, whereby the entire central aspect of the cornea was replaced by a donor cornea – a full-thickness transplant.
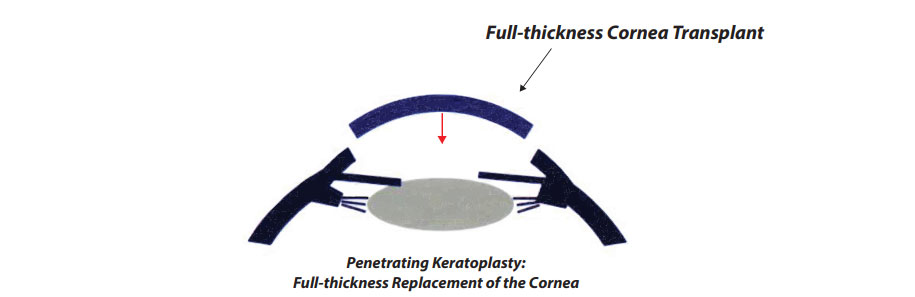
Today, several forms of newer transplantation procedures exist, and it is now possible to selectively replace different layers of the cornea, whilst retaining the unaffected layers. The major advantages to just replacing the diseased layers, and leaving the healthy layers untouched, include a stronger eye after surgery, better visual quality, faster visual recovery, and most importantly, a marked reduction in complications, both during and after surgery, which leads to a much higher success rate overall. These forms of partial thickness corneal transplantation are termed Lamellar Keratoplasty procedures.
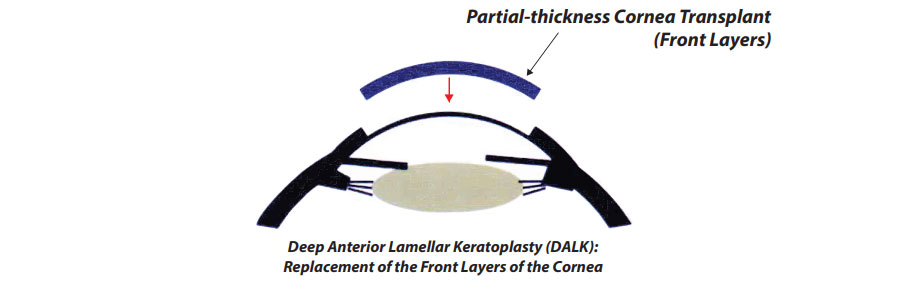
There are basically 2 forms of Lamellar Keratoplasty:
Anterior Lamellar Keratoplasty (ALK)
ALK procedures involve exchanging only the front layers of the cornea, leaving the innermost later (the Endothelial Layer), intact and unchanged. The commonest ALK procedure today is Deer Anterior Lamellar Keratoplasty (DALK), where all the front layers of the cornea are fully exchanged. The major advantaged of DALK is that the risk of corneal transplant rejection is greatly reduced to a 1-2% risk, compared to PK surgery, where the risk of rejection may be as high as 10%.
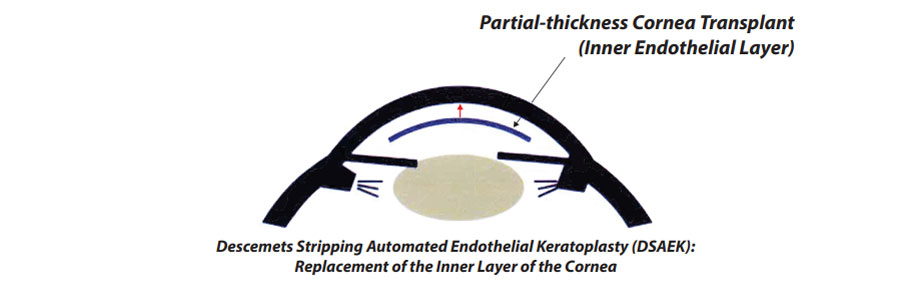
Endothelial Keratoplasty (EK)
EK procedures leave the front layers of the cornea intact, and instead exchange the innermost Endothelial Layer. Because the donor Endothelial Layer is usually inserted through a small side incision, there are no sutures on the cornea, and vision recovers much faster than PK or ALK. The risk of transplant rejection is also lower than PK, and ranges from 2-4%.
There are 2 forms of EK surgery, DSAEK (Descemets Stripping Automated Endothelial Keratoplasty), and DMEK (Descemets Membrane Endothelial Keratoplasty). The difference between the 2 procedures is the relative thickness of the donor tissue layer transplanted – in DMEK, the donor layer is the thinnest. Your surgeon will advise you which procedure will be more appropriate for your corneal condition.
ADVICE FOR PATIENTS UNDERGOING CORNEAL TRANSPLANTATION
Some facts about your corneal transplant operation:
Type of anaesthesia: Corneal transplants may be performed under either local anaesthesia (LA) (i.e. you will be given a numbing injection around your eye and will also be lightly sedated during the operation), or general anaesthesia (GA) (i.e. you will be fully asleep throughout the operation). PK and DALK surgery usually performed under GA, whereas DSAEK may be performed under with LA or GA – your surgeon will discuss which option is best for you.
Duration of surgery: this will depend on the exact type of corneal transplant, but surgery will usually last 1 to 2 hours, and you will usually be able to go home after surgery. Occasionally, you may be required to be admitted to hospital for one night after the operation.
Scheduling surgery: Corneal Transplantation requires suitable corneal donor tissue of the highest quality, which can only be obtained from an Eye Bank a few days prior to the surgery. FV Hospital partners with the Singapore Eye Bank, which is able to produce excellent quality corneal tissue which greatly assists in providing safer and more effective transplant procedures, which can result in a high success and visual quality.
Although the operation may have been scheduled days to weeks before, the final confirmation that your operation will proceed will depend on the final assessment of donor tissue quality which needs to occur 1 or 2 days before the surgery. It is therefore possible that your surgery may need to be postponed, if the donor is not suitable. However, if this occurs, you will be scheduled for the next available date for surgery, which is usually a few days later, once suitable donor tissue is available.
AFTER YOUR OPERATION
- Your eye may be red and tearing, and you may experience some mild discomfort for the first few days of surgery. This is normal, but if you are concerned, please let your surgeon know. Feel free to take paracetamol or ask for some mild painkillers.
- Immediately after a corneal transplant, a special form of soft contact lens, known as a bandage contact lens (BCL), is often placed over the new cornea to aid in rapid healing. Please ask your surgeon if you are not sure if a BCL was placed in your eye. The BCL will usually be kept in place day and night for several days to weeks after surgery, and does not need to be removed at night. Eye drops should be used as normal, over the BCL. Avoid eye rubbing to reduce the risk of dislodging the BCL. If it does come out, please do not attempt to replace it in the eye, and if you experience discomfort or tearing, please call for an earlier appointment at FV Hospital. At each postoperative visit, your surgeon will assess the need to keep the BCL in place, or to remove it once the eye has fully healed.
- In some forms of corneal transplantation (mainly lamellar keratoplasty procedures, i.e. DSAEK, DMEK, or DALK surgery) an air bubble is left inside the eye after the surgery to help keep the new transplanted corneal tissue in position. This air bubble will gradually dissolve over the next few days. If needed, you will be instructed to generally lie flat in bed, face upwards, for the first 24 hours after the surgery, so that the air bubble can continue to help keep the corneal tissue in place. Avoid using a pillow so that your face and eye is facing straight up towards the ceiling during this time. On the first postoperative day, your surgeon will usually inform you that it is no longer necessary to lie flat in bed with no pillow, but please ask if you are not sure. As the air bubble can expand in the eye in the first few days after surgery depending on atmospheric pressure, you will usually not be able to fly home for the first few days because of low cabin pressure, and if you are staying in a hotel, please avoid staying in a high floor (above the 20th), again to reduce the risk of air expansion.
- If your eye has stitches to hold the new cornea in place until full healing occurs, you need to take care that you do not accidentally hit the eye, and you should not rub your eye. The plastic eye shield which you will be provided with should be used for the first 2 weeks at night when sleeping, to prevent discomfort in bright sunlight for the first few days, and you may use sunglasses when outdoors, which will help alleviate any glare or discomfort. Avoid dusty environments and crowded areas for the first week. If you are concerned about water entering your eye during bathing, the careful use of swimming goggles when bathing which will largely prevent water entering the eye when you wash your hair or face. Avoid strenuous activities during the first month, although non-contact exercise (*such as walking, jogging, working out in the gym) can still be performed. Swimming is generally not advisable for at least the first 6 months after surgery. Please not that even after full healing, the eye after a corneal transplant is never as strong as before surgery, and all major contact sports should in general be avoided.
- Eye drops will always be prescribed after a corneal transplant, and these include antibiotic eye drops to prevent infection, and anti-inflammatory steroid eye drops which will not only reduce inflammation immediately after surgery, but are also absolutely essential to reduce the risk of corneal transplant rejection. Initially, these eye drops will need to be used every 3 hours during the day (approximately 5-6 times a day), but will gradually be reduced or tapered off over several weeks and months, depending on your eye surgeon’s instructions. In some forms of corneal transplant with a low risk of rejection, such as DALK surgery, eye drops may be able to be stopped by 4 to 6 months, but in most instances, eye drops will be needed for at least a year, and thereafter you may still require maintenance eye drops once or twice a day thereafter.
- After a corneal transplant, it is common that it will usually take a few days before your vision will start to improve and your vision will gradually improve over the first few weeks. However, your vision will usually only stabilize at about 3 to 6 months, depending on your type of corneal transplant, and will also be dependent on whether sutures need to be removed over the next few months. Once vision has stabilised, you will probably need to be prescribed spectacles or contact lenses to achieve your best vision. Occasionally, additional surgery in the form of graft refractive surgery may be required to reduce astigmatism.
- During the first few months, you will need to come for frequent follow-up visits at FV Hospital. Your surgeon will usually see you on the first day after surgery, and 2 or 3 more times within the first 10 days after surgery. If you have come to FV Hospital for the corneal transplant, and do not reside in Vietnam, you will need to plan to stay in Vietnam for about 10 days to 2 weeks after surgery, during which time you will be seen several times at the hospital. Thereafter you may travel home, but you will need to come back for a follow-up one month later. Thereafter you will need to come back for a follow-up every 2 to 3 months for the first year, and then come back yearly for follow-up visits after that.
COMPLICATIONS
In the ensuing weeks after a corneal transplant, your eye surgeon will need to ensure that complications do not arise, or are detected, and treated early. Common complications after a corneal transplant include corneal graft rejection, and raised eye pressure (glaucoma), both of which can be treated if diagnosed early. Sutures may also loosen early and cause infection.
1. The main complication after corneal transplantation is corneal transplant rejection, a condition where your body does not accept the new donor corneal tissue and your immune system attempts to reject, and damage the transplant. If diagnosed late, or left untreated, the corneal transplant may be permanently damaged, and a repeat corneal transplant will be required. If detected early however, corneal transplant rejection may be treated and reversed with the more frequent use of steroid eye drops, or oral steroid medications.
You should be aware of the early signs and symptoms of corneal transplant rejection, which are:
- Sudden eye pain or discomfort
- Sudden worsening of vision
- Sudden tearing and redness of the eye
These signs and symptoms may occur together, or singly, and if in doubt you should immediately contact FV Hospital for the earliest appointment possible. In a small percentage of cases, patients who are at a much higher risk of transplant rejection may be prescribed oral anti-rejection medications immediately after surgery, and for several months after surgery. As some of these medications have significant side-effects, your surgeon will discuss this with you in detail should the need arise.
2. Glaucoma, or raised eye pressure, is another possible complication occurring after a corneal transplant. At each visit with our specialists, your eye pressure will be checked, and if found to be high, glaucoma eye drops will be prescribed to lower the eye pressure, as prolonged periods of raised eye pressure (glaucoma) can result in permanent visual loss due to damage to the optic nerve, and you may be referred to a glaucoma specialist for co-management. In some instances, if eye drops or oral glaucoma medications fail to reduce eye pressure sufficiently, you may require glaucoma surgery to more permanently reduce the eye pressure.
3. Other complications which may arise after a corneal transplant include the premature loosening of sutures in the corneal graft, which may cause discomfort and lead to infection and these loose sutures will need to be removed by your eye surgeon in FV Hospital.
If you experience sudden tearing, discomfort, redness, or blurring of vision, or any combination of the above please contact the hospital immediately for an earlier appointment. When you call, please explain that you are a corneal transplant patient and that you need urgent consultation.
TAKING YOUR MEDICATIONS
- Please learn the names of all your medications and what they are for
- Please learn the doses and frequency of all your medications
- Please take all the medications as prescribed. If you experience discomfort, eye redness, sudden blurring of vision, or a skin rash, which could mean that you are developing an allergy to some of the medications, please contact us for an urgent appointment.
- Please take note of all the changes in your medications at each visit, as prescribed by your doctor
- Please inform the doctor if you are taking any other medications, or if you have any other medical illness
- Please do not miss a dose, or change the frequency of medications unless your doctor tells you to
- Please do not stop taking medications, simply because you “feel fine” – these medications are often preventing complications
- Please do not take any other form of “traditional medications” or “traditional remedies”, without first consulting your doctor
THE IMPORTANCE OF FOLLOW-UP VISITS AT FV HOSPITAL
After your corneal transplant, you will be given specific follow-up hospital visits – at each visit, our surgeon will check to ensure that your corneal graft remains healthy and clear.
Regardless of the type of corneal transplant performed, it is very important that you come for your scheduled appointment, so that any problems can be detected early, and that you continue to receive the best treatment and care to ensure that your corneal transplant continues to be successful.
Although follow-up appointments will initially be frequent, these will be tailed down over the next few months, once the transplant is stable and has healed well. The first year after a corneal transplant is the most crucial period after surgery, but because there will also be a lifelong risk of transplant rejection, life-long yearly follow-up remains important.



