
WHAT IS GESTATIONAL DIABETES?
Gestational diabetes is a type of diabetes that develops during pregnancy (gestation) in women who have never had high blood sugar before. Having diabetes means the amount of sugar in your blood is higher than it should be.
Gestational diabetes usually:
- Develops in the second half of pregnancy;
- Is controlled by eating healthy foods, exercising and, if necessary, taking medication;
- Goes away soon after your baby is born.
WHAT CAUSES GESTATIONAL DIABETES?
When you eat, some of your food is broken down into sugar (also called glucose). Sugar travels in your blood to all of your body’s cells. The cells use sugar for energy. Insulin helps sugar move from your blood into your cells. Insulin is a hormone that is made by the beta cells in your pancreas.
When you have gestational diabetes, weight gain and the effect of pregnancy hormones made by the placenta can cause a resistance to insulin in your body. Your body tries to produce more insulin to handle the extra sugar, but it is still not enough. So the sugar stays in your blood instead of moving into your cells. That’s why the sugar levels in your blood get too high.
HOW CAN GESTATIONAL DIABETES AFFECT ME AND MY BABY?
During pregnancy, when you have high blood sugar, your baby will have high blood sugar too. Your baby’s body responds by making extra insulin to move the sugar into the body cells. The baby is able to use this extra sugar by storing it as fat. This makes your baby grow larger. Extra sugar can impair the development of your baby’s lungs, liver and other organs.
Your baby’s growth will be measured using ultrasound. If your baby is large, a vaginal birth can be more difficult and you may need a C-section. Your doctor or midwife will discuss your risks around the time of delivery, when they know the size of your baby.
After birth, your baby is no longer affected by your high blood sugar level. However, the extra insulin your baby was used to making continues to work. This could lead to a drop in his or her blood sugar initially after birth. Your baby will be closely watched and treated for low blood sugar if needed.
Women with gestational diabetes that is not carefully managed can have uncontrolled blood sugar levels and might have:
- A higher chance of needing a C-section
- Miscarriage
- High blood pressure or preeclampsia
- Pre-term birth
- Future diabetes.
HOW IS GESTATIONAL DIABETES TREATED?
It is essential to monitor and control your blood sugar to keep your baby healthy and avoid complications during pregnancy and delivery.
Controlling your blood sugar:
- Makes you feel healthier and less tired;
- Lowers the chances of having a very large baby with serious health problems;
- Keeps your baby’s blood sugar at a healthy level after birth.
Most women with gestational diabetes can control their blood sugars just by making simple changes in their diet along with physical activity (see below). Healthy eating is the most important way to have a healthy pregnancy and baby.
For some women, healthy eating and physical activity are not enough to control their blood sugars. If your blood sugars stay high, you may need to take insulin.
The dietitian will help you make a plan for healthy eating. Eating well gives you the nutrients you need to feel good, have energy and support a healthy pregnancy.
Your plan will include:
- Avoiding foods that are high in sugar;
- Eating smaller, more frequent meals;
- Eating the suggested amount of carbohydrate in your meals and snacks.
Carbohydrates (sugar, starches and fibre) are sources of energy found in a variety of foods. Most carbohydrates breakdown into sugar (glucose). You need to eat carbohydrates for good health and a healthy pregnancy. However, eating too much carbohydrate will raise your blood sugar.
How healthy eating helps control your blood sugar levels
- Limiting the amount of sugar/ carbohydrate in a meal or snack.
- Limits the amount of blood sugar that your body has to cope with at that time.
- Blood sugars are better controlled.

HOW SHOULD I EXERCISE?
During your prenatal visits, your doctor and your midwife will talk about physical activity during pregnancy.
Regular physical activity plays a key role in every woman’s wellness plan before, during and after pregnancy. Exercise lowers your blood sugar by stimulating your body to move glucose into your cells, where it’s used for energy. Exercise also increases your cells’ sensitivity to insulin, which means your body will need to produce less insulin to transport sugar.
As an added bonus, regular exercise can help relieve some common discomforts of pregnancy, including back pain, muscle cramps, swelling, constipation and trouble sleeping. Exercise can also help get you in shape for the hard work of labour and delivery.
With your doctor’s approval, aim for moderately vigorous exercise on most days of the week. If you haven’t been active for a while, start slowly and build up gradually. Walking, cycling and swimming are good choices during pregnancy. Everyday activities such as housework and gardening also count.
HOW OFTEN SHOULD I TEST MY BLOOD SUGAR?
We will give you a blood sugar monitor, show you how to test your blood sugars and record them in your Diabetes Record Book.
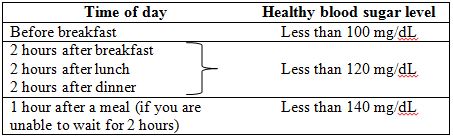
Test your blood sugar four times a day. Write down each result in your Diabetes Record Book. Match it with the “target” blood sugar levels in this chart.
Bring your Diabetes Record Book and monitor to all your appointments.
HOW WILL MY BABY MONITORED?
An important part of your treatment plan is close observation of your baby. Your doctor may monitor your baby’s growth and development with repeated ultrasounds or other tests.
If you don’t go into labour by your due date – or sometimes earlier – your doctor may induce labour. Delivering after your due date may increase the risk of complications for you and your baby.
WHAT HAPPENS AFTER I HAVE MY BABY?
Gestational diabetes usually goes away soon after your baby is born. In the hospital, your blood sugar will be checked to see if it has returned to normal.
When you have finished breastfeeding or six weeks after you deliver, your family doctor will arrange a glucose tolerance test. This is the same blood test that you had during pregnancy. The results will show if you continue to have diabetes.
WILL I GET DIABETES IN THE FUTURE?
Having gestational diabetes makes it more likely that you will develop diabetes in your next pregnancy or later in life.
To lower the chance of getting diabetes in the future:
- Breastfeed your baby;
- Continue healthy eating;
- Keep your weight at a healthy level;
- Exercise regularly.
Talk with your doctor about what you can do to stay healthy, for yourself and your baby!



