This document has been conceived under the authority of the French Society of Plastic Reconstructive and Aesthetic surgery (Société Française de Chirurgie Plastique Reconstructrice et Esthétique – SOFCPRE) to complete the information that you received in your first consultation with your Plastic Surgeon. It aims to answer all the questions that you might ask, if you decide to undertake mammoplasty.
The aim of this document is to give you all the essential information you need in order to make an informed decision, with full knowledge of the facts related to this procedure. Consequently, we strongly advise you to read it carefully
DEFINITION, AIMS AND PRINCIPLES
Mammary hypoplasia is defined as a breast volume which is insufficiently developed in proportion to the patient’s morphology. It can be a pre-existing condition (small breasts from puberty) or appear later, after substantial weight-loss, a pregnancy followed by breast-feeding, or hormonal problems.
It can occur alone or be associated with ptosis, that is sagging of the breasts and skin stretching and a lowered areola.
This insufficient breast volume is often a source of physical and psychological distress for the patient who feels she lacks femininity, and also a lack of self confidence and poor self-image which can lead to an inferiority complex. Breast augmentation with implants is the solution to these problems.
The procedure can be carried out at any age above 18
Below this age the procedure is not advisable.
This is a purely cosmetic procedure and cannot be reimbursed by health insurance; Only rare cases of total absence of breast formation (mammary agenesis) can be partly reimbursed after prior agreement.
The implants used at present are composed of a shell and a filler.
The shell is always made of silicone rubber, but the filler can vary, which means the filler inside the shell.
The implant is termed ‘pre-filled’ when the filler was inserted during the manufacturing process (gel and/or saline solution). The different volumes are therefore fixed by the manufacturer.
Implants filled with saline solution are filled by the surgeon who can adapt them to the patient to a certain extent during the procedure.
New generation pre-filled silicon gel implants
The great majority of implants used in France and elsewhere in the world are pre-filled silicon gel implants.
These implants, which have now been used for over 40 years have been proved to be safe and to be the best product for this procedure since they are very close to the consistency of a normal breast. There has been great progress in this domain since the late 1990’s, any weak points have been eliminated. At present all implants available in France have been certified as safe by the EU and the French health and safety agency (Afssaps).
They are made of soft silicon gel inside a strong impermeable envelope of silicone rubber which can be rough or smooth.
The most important points concerning the new generation of implants, which ensure their safety, are the new improved envelopes and the gel itself.
- The shells, which are now stronger, prevent any leakage of gel (which was a cause of capsule formation) and have much greater resistance over time;
- Cohesive silicone gel which has a thicker consistency will not spread in case of rupture of the envelope.
Added to this increased reliability is the fact that this new generation of silicon implants exists in different shapes, making it possible to adapt them to individual needs. Thus in addition to the classic round implants, anatomic ‘teardrop’shapes which can be higher, wider or more pointed.
This diversity of shape, associated with a range of volumes means that the choice of implant can be tailored to the figure and the expectations of the patient
Other types of implants
The envelopes are always silicone rubber, it is the filler which can be different. At present in France only two alternatives to silicone gel are authorized:
Physiologic saline : This is in fact salt water (which makes up 70% of the human body). These implants can be ‘pre-filled’ by the manufacturer or ‘inflatable’, that is, filled by the surgeon during the procedure. Since the filler is a liquid rather than a gel the breasts do not feel natural, the implants can wrinkle, which can be palpable or even visible; They can also deflate suddenly even after a short time.
Hydrogel: This is the latest substance authorized (in 2005) by the French regulatory agency. It is a water-based gel mainly composed of water and a cellulose-based product. This gel, with a more natural consistence than saline solution, can in the same way be absorbed into the body in case of leakage from the shell
BEFORE THE PROCEDURE
After discussion between the patient and the physician who will have clearly explained the different options, the best choice for each case is agreed during the preoperative consultation, taking into account all the relevant parameters ( height, weight, pregnancies, breast feeding, body shape, body fat, size of the existing breasts, muscle tone…).
After studying these parameters and anatomic features of the patient, the surgeon will determine the plan for the operation. This will also take into account his preferred technique and the expectations of the patient and the positioning of the scars, the type and size of implants, and the position of the implants above or below the muscle. A thorough preoperative examination with blood tests will be carried out as prescribed (re: see further).
A blood test will be performed accordingly with the prescriptions
An anesthesiologist will see you in consultation at the latest 48 hours before the operation.
In addition to the usual preoperative tests it can be helpful to use medical imagery (mammography, echography)
No aspirin-based medication should be taken during the 10 days preceding the operation
You will probably be asked not to eat or drink anything for six hours before the operation
HOSPITAL STAY AND TYPE OF ANESTHESIA
Type of anesthesia: This is usually classic general anesthesia, you will sleep throughout the operation. Rarely ‘twilight’ anesthesia is used (local anesthesia with intravenous sedation), this can be discussed with the surgeon and anesthesiologist
Hospital stay: One day in hospital is usually sufficient. The patient arrives in the morning (or the previous afternoon) and leaves the next day
However the procedure can be carried out in an ambulatory setting, the patient leaves after some hours of medical supervision
THE PROCEDURE
Each surgeon has adopted his or her own specific technique, which he or she adapts in order to obtain the best results in each case. We can however give some basic points:
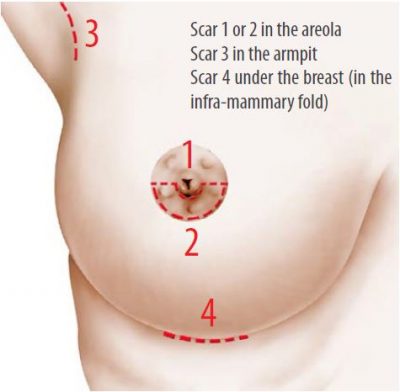
The incisions
There are several possible approaches:
- Peri-areolar approach(around the areola) the incision is either below the circumference of the nipple or horizontal to the nipple (1&2);
- Axillary approach, the implant is inserted through a small incision located in the armpit (3);
- The infra-mammary approach, the incision is in the infra-mammary fold (4).
These incisions correspond of course to the position of future scars which will thus be hidden in natural folds or lines.
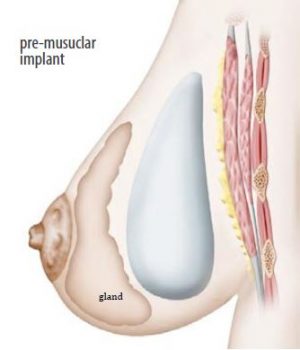
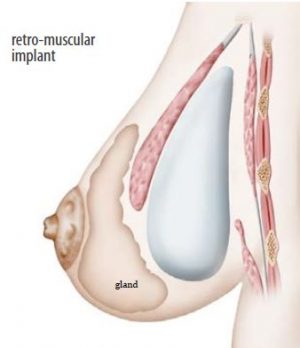
The position of the implant
Through these incisions, two positions are possible:
- This can be in a pocket made in the breast tissue behind the mammary gland and in front of the pectoral muscle,
- or behind both the mammary gland and the pectoral muscle.
- The choice of position will be determined in consultation with the surgeon.
Additional surgery
In case of ptosis (sagging breasts, a lowered areola), it is appropriate to associate a breast lift (mastoplexy); this implies additional larger scars (around the nipple, or in a vertical position)
Dressings and drains
A drain may be left in place for a few days after the procedure in order to evacuate any blood or liquid which may form around the implant
At the end of the procedure an elastic bra-like bandage is put in place.
The length of the procedure varies with each surgeon and of course lasts longer with additional surgery but in general the operation lasts one to two and a half hours.
AFTER THE OPERATION: POST-OPERATIVE EFFECTS
There can be pain for the first few days after the procedure, particularly when the implant is large and/or placed behind the muscle. In this case pain medication of the strenth necessary to dull the pain, is prescribed for several days. Even if there is no pain there will be a strong sensation of tightness.
Swelling and bruising of the breasts, and difficulty in raising the arms are frequent immediately after surgery.
The original dressing is removed a few days after the procedure and is replaced by a lighter dressing, then an elastic bra can be recommended to be worn night and day for a few weeks
If the stitches are non-absorbable they will be removed several days after surgery.
Five to 10 days convalescence is necessary before returning to work.
Patients are advised to wait for one to two months before practising any sports
THE RESULT
This can be truly seen from two to three months after surgery, the time necessary for the breasts to become softer and for the implants to settle
The procedure will improve not only the volume but the shape of the breasts. The scars are usually hardly visible. The added breast volume affects the figure in general, this means that more elegant clothes can be worn. Added to this aesthetic improvement there is usually a positive psychological effect due to enhanced femininity.
The goal of this surgery is to make an improvement and not to achieve perfection. If your wishes are realistic, the result should give you great satisfaction.
Duration of results
The implants have their own life-span, (see below) but without taking this into account the result of this procedure concerning volume, is long-lasting.
The exception can be when a patient puts on a lot of weight. It is true however the shape and firmness of the ‘enlarged’ breasts will sufer, like ordinary breasts, from the effects of aging and gravity which cause drooping, more or less rapidly according to age and support quality of the skin, and also the volume of the implants
Disappointing results
The following problems can occur occasionally:
- Asymmetry of the final volume in spite of the use of different sized implants to correct the problem.
- Stiffness with insufficient softness and mobility (especially with larger implants).
- An artificial appearance especially for very slim patients, the upper limit of the implant is visible
- The implant can be detected when touched especially when the thickness above the implant is reduced (skin + fat + gland) and when the implant is large
- Aggravation of a mammary ptosis can be observed especially when using a large implants
In cases where the patient is not satisfied with the result certain problems can be corrected by revision surgery after a few months
FREQUENTLY ASKED QUESTIONS
Pregnancy/breastfeeding
After having this procedure there is no problem regarding pregnancy either for the mother or the child, but it is advisable to wait for six months after surgery. Breast feeding is still possible in most cases.
Auto-immune disease
Many international research papers published on the subject have shown that there is not a higher risk of contracting this type of rare disease with implants compared to the general female population.
Implants and breast cancer
To our knowledge at present we can confrm that breast implants, including those filled with silicone, do not increase the risk of breast cancer.
However, during screening techniques clinical examination and palpation can be affected, especially in case of siliconoma or capsular contraction. The presence of the implants can also make it difficult to carry out and read routine mammographies. It is necessary to explain beforehand that you have implants. Other radiological techniques can be used; echography, MRI etc. Furthermore, if there is doubt as to a diagnosis of breast cancer you must be aware that more invasive exploratory techniques may be used in order to be sure of the result
How long will the implants last ?
Although it is true that some patients can keep their implants for decades without major changes, an implant, whether filled with silicon gel or saline, cannot be said to last for a specific time, this is not a permanent life-long prothesis. A patient with implants must expect them to be replaced at some point in time, if the initial effect is to be maintained. It is impossible to predict the life-span of an implant, of whatever type, as this depends on wear which is variable. This means that no guarantee can be given regarding their life-span
It should be noted however that the new generation implants are far more hardwearing and reliable. The notion of replacement after ten years is no longer justified, they only need to be replaced if a problem is detected, or the patient wishes to change their size or shape or to correct ptosis.
Follow up
It is important to keep the appointments with your surgeon during the weeks and months following the operation. After this stage regular medical visits with, for example your gynecologist, or for routine mammography will continue this follow up. You must tell each physician that you have breast implants
A specific visit concerning the implants is advisable every two to three years, but in case of a change observed in a breast, or an accident affecting the breasts, an appointment must be scheduled
POSSIBLE COMPLICATIONS
Breast augmentation with implants, although essentially an aesthetic procedure, is nevertheless an operation, and this implies that the risks inherent to any surgery apply here.
A distinction should be made between risks related to the Anesthesia and those related to the surgery:
- For the anesthesia, the anesthesiologist will explain the risks during the preoperative You must be aware that anesthesia can cause unpredictable reactions, which can be difficult to control: the presence of an experienced anesthesiologist, in a surgical context, means that the risks are statistically practically negligible.
In fact, techniques, products and monitoring methods have progressed considerably over the last twenty years, giving optimal safety, especially when the surgery is elective and the patient is in good general heath.
- Concerning surgery: by choosing a competent, qualified Plastic Surgeon, used to performing this procedure, you limit the risks to a large extent, without however eliminating them completely.
In general after augmentation mammoplasty the recovery period is straight forward. There can however be complications some of which are inherent to all breast surgery, some linked to the placing of a foreign body in the breast: that is to say risks linked to implants
Possible complications inherent to all breast surgery:
Effusion, infection
- A hematoma: blood can surround the implant shortly after surgery. In case of heavy bleeding it is necessary to return to the operating room to drain the blood and put a stop to the bleeding
- Serious effusion: this means an accumulation of lymphatic liquid around the implant. It is a frequent complication often associated with considerable swelling. It rises to a temporary increase in the volume of the breast or breasts. It decreases gradually and disappears
- Infection: rare after this procedure. It can require more than one course of antibiotics and the removal of the implant for several months following drainage (after this time interval another implant can be put in place).
Three types of infection exist:
- Late (silent) infection: this has few symptoms and can occur several years after implantation.
- A microabcess: more frequent than the above, they can form on stitches and are absorbed after their removal with local treatment.
- Toxic shock syndrome: rare cases of this have been reported
- Skin necrosis: this occurs when tissue is starved of oxygen due to interruption of blood supply to the zone involved. This can be favored by high blood pressure, hematoma, an infection or heavy smoking by the patient. It is a rare complication but is formidable as, if serious, it can reveal the surface of the implant, notably by splitting the stitches. A second operation is often required, with possibly the need to remove the implant
- Abnormal scar: formation the healing process is unpredictable and scars can be less discreet than expected. They can be widened, retractile, hyper- or hypo-pigmented, hypertrophic, or rarely, cheloid o ciété
- Sensory changes: this is frequently found in the first few months but usually diminishes over time; Rarely however, a certain degree of dysesthesia (heightening or diminution of sensitivity) can persist around the areola and the nipple.
- Galactorrhea/milk secretion: very rare cases of unexplained postoperative hormonal stimulation have been reported, giving rise to milk secretion which sometimes collects around the implant.
- Pheumothorax: very rare, has specific treatment.
Specific implant-related risks
- Wrinkling or rippling: the implant is soft and natural, and for this reason the outer envelope of the implant can form creases, which can be palpable or visible in certain positions under the skin, giving a ‘ripple’, effect
- Capsular contractures: it is a normal physiological reaction that a fibrous shell should develop around an implant. A normal reaction to the presence of a foreign body in the organism is to isolate it from the foreign body with a hermetic membrane called a ‘periprosthetic capsule’. Normally this membrane is thin, supple and imperceptible but the reaction can increase and the capsule can thicken, become fibrous and contract exerting pressure on the implant, it is then known as a ‘capsule’. There are four stages of hardening that range from a normal undetectable aspect to severe forms giving hard, round, immobile breasts which can be painful.
Capsular contraction can follow infection or a hematoma, but often has no determined cause, resulting from unpredictable organic reaction
Surgical techniques have made great progress in recent years, but especially the design and products used for the implants are much improved, this means a considerable reduction in the number of cases of capsular contraction and their seriousness. If necessary, the capsule can be incised in a surgical procedure (capsulotomy).
- Rupture: we have seen that implants have a limited life-span. An implant can become porous and the silicone rubber envelope of the implant can deteriorate. It can become porous, have tiny leakages or split. This can be rarely after an accident, a puncture with a needle or because of a manufacturing flaw. Much more often, however this is due to deterioration of the implant over time
In all cases this will result in a leakage of the filling product, with different consequences according to the product:
- If the implant is filled with physiologic solution or resorbable hydrogel the implant will deflate partially or totally, either suddenly or slowly.
- With silicone gel (non-resorbable) this will remain inside the membrane surrounding the implant.
This can cause capsule formation or can remain unnoticed.
In some cases, much rarer now, (mainly because the modern gels are more cohesive), the gel can penetrate the surrounding tissue.
Rupture of the implants usually requires an operation to change them.
An incorrect positioning or secondary displacement of implants, while affecting the shape of the breast, can sometimes justify surgical correction.
Although rare in practice, the turning of an “anatomic” implant remains theoretically possible and could affect the cosmetic result.
- Deformation of the chest wall
In rare cases, implants with fibrous capsules, left in place for a long period of time, can make an “imprint” in the tissues, leaving, when removed, a distortion of the chest wall that is difficult to correct.
Tell us what you think.
These booklets are regularly reviewed.
We welcome any suggestions to help us improve this booklet. You should send these to Patient and Family Eduacation Commitee, Fv Hospital, 06 Nguyen Luong Bang Street, Saigon South (Phu My Hung), District 7, Ho Chi Minh City, Vietnam
E-mail: patient.eduacation@fvhospital.com