Surgery Of Breast Reduction Or Mammaplasty
This document has been conceived under the authority of the French Society of Plastic Reconstructive and Aesthetic surgery (Société Française de Chirurgie Plastique Reconstructrice et Esthétique – SOFCPRE) to complete the information that you received in your first consultation with your Plastic Surgeon. It aims to answer all the questions that you might ask, if you decide to undertake plastic surgery for mammary reduction.
The aim of this document is to give you all the essential information you need in order to make an informed decision, with full knowledge of the facts related to this procedure. Consequently, we strongly advise you to read it carefully.
Definition
Mammary hypertrophy is an increase in the volume which is much more than the normal of the breast, especially in comparison with the patient’s morphology. Such an excessive volume of the breast often causes the breast to be sagged or drooped too much (ptosis mammary) and sometimes asymetric at some certain degree.
Mammary hypertrophy can cause many physical and functional problems (neck, shoulders and back pain, difficulties when practicing sports, when dressing). Mammary hypertrophy also causes notably psychological impact. These problems justify why health insurance companies should cover them.
Objectives
The surgical intervention aims at reducing excessive breast volume, correcting ptosis mammary and asymmetric breasts in order to obtain a pair of breasts that are harmonious with the patient’s morphology (reduced, lifted, symetrised and re-shaped pair of breasts).
Principles
The operation is performed for ablation of excessive mammary gland tissue and for preserving a breast volume that is harmonious with the patient’s silhouette and conforming with her wishes. The residual glandular volume is lifted, concentrated and re-shaped.
The cutaneous covering will then be adapted, which means the excess skin is removed in such a way that ensuring beautiful curve for the new breasts. Thus, the cut banks of the skin are then sutured: The sutures are the origin of the scars.
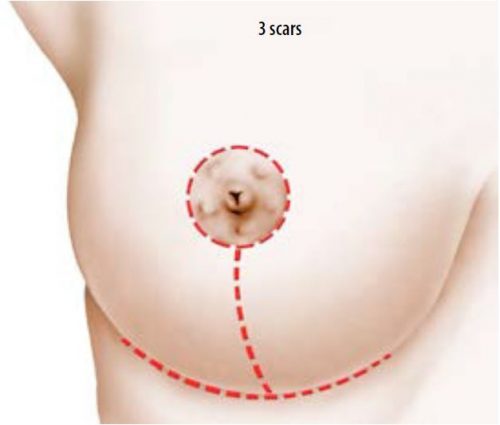
Most of the time the scar is in the shape of an up side down T with 3 parts: peri-areola, to the circumference of the areola between the brown and the white skin of the breast, vertical, between the lower pole of the areola and the sub mammary furrow, horizontal, concealed inside the sub mammary furrow.
The length of the horizontal scar is proportional with the size of the hypertrophy and the ptosis.
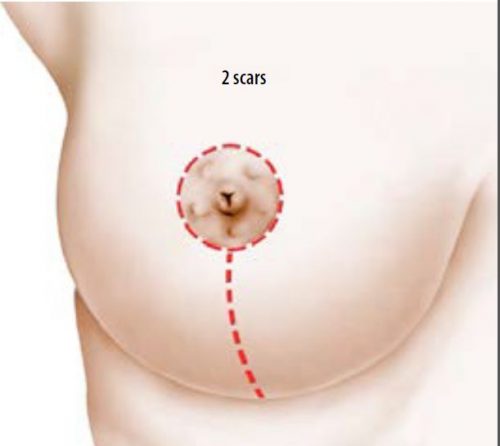
In some cases, especially moderate mammary hypertrophy and ptosis, a method called “vertical” which allows the transversal scar inside the sub mammary groove to be avoided and the scar at the peri-oreola and vertical parts to be reduced.
Plastic surgery for mammary hypertrophy can be carried out at the end of and beyond the growth stage and during one’s lifetime.
Later pregnancy is obviously possible and so is breast feeding, but it is advised to wait at least 6 months after the operation.
This operation does not increase the risk of cancer.
BEFORE THE OPERATION
Normally, a pre-operative test will be done according to prescription.
An anesthetist will provide you with a consultation at least 48 hours before the operation.
Besides the normal pre-operative examinations, it can be helpful to verify the mammary images (mammography, echo-graphy).
It is recommended to stop smoking, at least one month in advance or one month after the operation ( tobacco can be the cause of a healing delay).
Stopping of an eventual oral contraception can be required, especially when associated risks are involved (obesity, bad venous status, coagulation disorders).
Any medicine containing aspirin should not be taken in 10 days prior to the operation.
Types of anesthesia and hospitalization mode
Types of anesthesia: This is classic general anesthesia, during which you will sleep deeply.
Hospitalization: Normally, hospitalization of 1 to 3 days is necessary.
The procedure
Every surgeon adopts a technique that is proper and adapts to each case to obtain the best results. However, the following basic principles should be retained:
The removed tissues must be systematically sent to a specialised laboratory to be microscopically examined (histological examination).
At the end of the operation, a shaping dressing with elastic strips in the form of a bra is made;
Depending on the surgeon and the size of the hypertrophy, the operation can take 2 to 4 hours.
After operation: Post-operative effects
The post-operative effects are generally a little painful and simple pain relief medicines are necessary.
Inflation (edema) and ecchymosis (blue) of the breasts, and troubles elevating the arms are frequently noticed
The first dressing is removed after 48 hours and replaced by a lighter one, forming a kind of elastic long-line bra made on measurement.
Being discharged in 1 to 3 days after the intervention, the patient is reviewed in follow-up consultation in 2 to 3 days after that.
Wearing a bra in place can ensure a good tension.
This kind of bra is advised to be worn in about a month, night and day, during the recovery stage.
If the surgical threads are not resorbable, they will be removed in 8 to 20 days after the operation.
It is advisable to envisage convalescence and stop working in 8 to 15 days.
It is advised to wait from one to two months before resuming sport activities.
The result
The result can only be judged 1 year after the operation: the breasts often have harmonious curve, and are symmetric or nearly symmetry, and natural. Besides such an improvement, the intervention has good impacts on the weight balance, practice of sports, dressing and psychological state.
It is advised to simply have patience to wait for a necessary time for the scars to be lessened and abide by a good monitoring during this period, and take a consultation every three to six months in a year. The operated breast is natural and especially sensitive with hormonal changes.
The objective of this operation is to provide an improvement not a perfection. If your wish is realistic then the acquired result should give you satisfaction.
Imperfective result
It is mainly to follow-up the scars carefully: the scar often appears to be pink and swollen in 2 to 3 months after the operation. After this period, these scars will gradually shade off with time, and become faintly visible. However, the scars may be large, white or, in contrary, brown.
It is necessary to know that the scars will shade off with time but they do not completely disappear. Regarding this matter, it should be remembered that surgeon is the one who sutures but patient is the one who heals the scars.
In some cases, the breasts can be asymmetric in terms of the volume, height, size or orientation of the areola.
In all cases, the asymmetries can be corrected with a secondary surgery but it should be at least 1 to 2 years later.
Possible complications
Surgical mammary reduction, although applied for aesthetic purpose, is also a real surgical intervention that involves the risks pertaining to all medical actions, however minor it is.
It is necessary to distinguish complications caused by anesthesia and complications caused by the surgery.
- Regarding anesthesia, upon providing consultation, the anesthetist shall inform the patient about the risks of anesthesia. It is known that anesthesia induces unpredictable reactions which are hard to control in the body: anesthesia provided with perfectly professional competence, in a real surgical background makes the risks statistically negligible.
It should be known that indeed the techniques, the anesthetic products and the follow up methods have progressed excellently during the last 20 years, offering an optimal safety, especially when the operation is not performed as an urgency and is practiced on a healthy person.
- Regarding surgical actions: choosing a qualified and competent plastic surgeon that is trained for this type of operation, you can minimize the risks, although not completely avoid them.
Happily, the complications rarely occur in plastic mammary reduction performed correctly. In reality, the majority of the operations are performed without problem and the patients are thoroughly satisfied with the results.
As such, and despite of the low frequency, you still need to know the possible complications:
- Thromboembolic accidents (phlebitis, pulmonary embolism), although these complications are really rare after this kind of operation, they are among the most fearsome ones. Strict preventive measures to minimize the accidents: wearing anti-thrombosis stockings, getting up early depending on the anti-coagulation treatment.
- Infection occurrence needs to be treated with antibiotics and surgical drainage in some cases;
- Hematoma may require an evacuation;
- Delayed healing can sometimes be observed, which prolongs the postoperative course.
- Necrosis of the skin or gland, in fact rarely seen with modern techniques, may be responsible for delayed healing (the risk is increased by smoking).
- Alterations in sensitivity, including the nipple, can be observed, but normal sensitivity usually returns within 6 to 18 months.
- Especially, the evolution of scars may be unfavourable, due to the occurrence of hypertrophic scars or keloids, of unpredictable onset and evolution, which can compromise the aesthetic outcome and require specific local treatment, often of long duration.
Thus, in the vast majority of cases this procedure, if well studied previously and properly performed, gives a very pleasant result in terms of comfort, even if the scarring is inevitable and the main drawback.
All things considered, the risks must not be overestimated, but you must be conscious that an operation, even a minor one, always has some degree of unforeseeable unknown factors.
You can be assured that if you are operated on by a qualified Plastic Surgeon, he will have the experience and skill required to avoid these complications, or to treat them successfully if necessary.
Tell us what you think.
These booklets are regularly reviewed.
We welcome any suggestions to help us improve this booklet. You should send these to Patient and Family Eduacation Commitee, Fv Hospital, 06 Nguyen Luong Bang Street, Saigon South (Phu My Hung), District 7, Ho Chi Minh City, Vietnam
E-mail: patient.education@fvhospital.com