The brachytherapy technique allows precise targeting of tumours, delivering a high dose of radiation to eliminate cancer cells without damaging healthy tissues in the body.
Hy Vong Cancer Care Centre, led by Dr Basma M’Barek, offers the brachytherapy technique for gynaecological cancer treatment at FV Hospital, and reports that the response in patients is highly positive.
Brachytherapy allows the complete elimination of cervical uterine tumour.
After experiencing several months of abnormal vaginal bleeding, Patient Trang (44 years old, from Quang Ngai province) visited a major hospital in Ho Chi Minh City for examination. Doctors there conducted a biopsy and concluded that she had cervical cancer.
Ms Trang was shocked and couldn’t believe her diagnosis. Two months prior, the results of her general health check-up and Pap smear screening for cervical cancer at another hospital in Ho Chi Minh City had been normal.
In October 2022, she decided to seek consultation and treatment at FV Hospital. Dr Basma M’Barek, Head of Hy Vong Cancer Care Centre, FV Hospital, examined Ms Trang and diagnosed cervical cancer at FIGO stage 2B, which is an intermediate stage.
Early-stage cervical cancer can be effectively treated through surgery. However, at this intermediate stage, cancer cells have already invaded a part of the vagina. As a result, the optimal treatment approach is a combination of radiation therapy and chemotherapy.

The Elekta Infinity digital linear accelerator at Hy Vong Cancer Care Centre.
Dr Basma designed a combined treatment protocol for Ms Trang, involving external and internal radiation therapy over a span of five weeks. Her regimen included five sessions of chemotherapy and 25 sessions of external radiation therapy to eliminate cancer cells in the uterus, vagina, and surrounding lymph nodes. Dr Basma and her team delivered radiotherapy via the advanced Elekta Infinity digital linear accelerator, equipped with VMAT technology to enable precise delivery of radiation to tumour masses while minimising damage to surrounding healthy tissues.
After completing the course of treatment, results showed that Ms Trang had responded positively to radiation therapy with an 80 per cent improvement in her condition. At this point, Ms Trang received brachytherapy, also known as internal radiation therapy, to eradicate the remaining tumour cells.
“Brachytherapy is a technique deployed in close proximity to the tumour to effectively eliminate cancer. A device is placed inside the patient’s body to deliver a radiation source directly to the tumour area. As a result, the radiation does not pass through healthy organs in the body, reducing side effects, while also allowing a high concentration of radiation to be directed at cancerous cells, thus shortening the treatment time,” explains Dr Basma.
In Ms Trang’s case, brachytherapy helped to preserve the uterus and the organs affected by the tumour. After the brachytherapy sessions, tests revealed that her cancer had been completely eradicated. During a follow-up examination in June 2023, Ms Trang’s health was normal, with no signs of remission.
Brachytherapy: Why is it highly effective but not widely adopted?

Elekta Flexitron brachytherapy remote afterloader at FV Hospital
FV Hospital implements brachytherapy in the treatment of various gynaecological cancers. Over the past year, Hy Vong has treated more than 10 cases of cervical cancer using brachytherapy, most of which have shown positive outcomes.
Aside from the advantages of direct, accurate targeting of the tumour, brachytherapy also reduces the risk of recurrence and shortens the duration of treatment. For instance, breast cancer patients typically require three to five weeks of external radiation therapy after mastectomy, whereas utilising brachytherapy immediately after surgery might mean only five days of radiation is needed to treat early-stage cases.
Despite its numerous benefits, not all cancer treatment centres around the world apply the brachytherapy approach. In Ho Chi Minh City, only two hospitals offer this method.
Dr Nguyen Huynh Ha Thu, MD, PhD, Hy Vong Cancer Care Centre, FV Hospital, explains that the radioactive sources used in brachytherapy decay continuously decay, even when not in use on patients. Therefore, infrequent usage of the equipment can create economic pressures.
“FV Hospital has adopted the brachytherapy technique as we aim to provide a comprehensive array of tools in the fight against cancer, ensuring that patients receive the best treatment protocols. Many oncology centres want to incorporate brachytherapy in patient care but can’t always afford to: FV Hospital will collaborate with our colleagues at other hospitals or specialist clinics when they need to employ brachytherapy for their patients. We strive to be a leading institution in the field of brachytherapy among private hospitals,” says Dr Basma M’Barek.
Brachytherapy at FV: Tailored treatment protocols for each patient
When applying the brachytherapy technique, radiation doses are administered on a weekly basis. However, the timing and frequency of radiation need to be tailored according to each patient’s unique condition to achieve optimal effectiveness.
Dr Basma says that rather than following a standardised protocol, FV doctors design radiation treatment plans based on specific indicators for each patient, considering their organ size, medical history, and disease status. Furthermore, each radiation session will be recalibrated according to the patient’s current condition on any given day. The goal is to optimise the radiation dose and target cancer cells precisely to eliminate them without harming surrounding healthy tissues.
Simultaneously, the doctors will also calculate treatment schedules and costs to optimise patient travel and expenses. Treating cancer not only contributes to the patient’s well-being but also provides psychological comfort and improves the quality of life after treatment for both the patient and their loved ones.
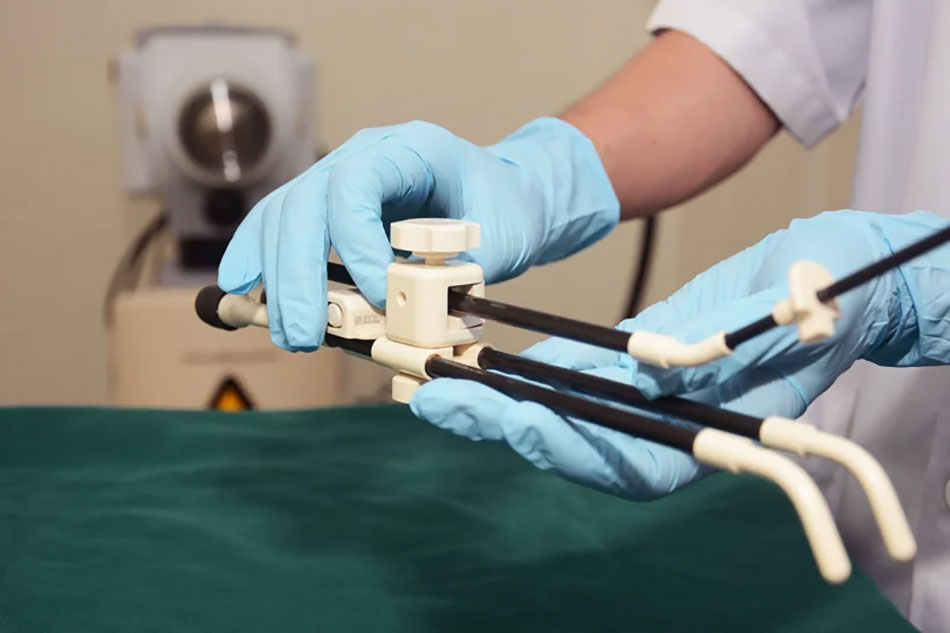
The set of instruments containing the radiation source will be directly inserted into the area impacted by the tumour inside the body.
At FV, the placement of the radiation-emitting device through the vaginal route to access the tumour in the cervix is performed by specialist oncologists who have received extensive training in brachytherapy. This procedure is conducted under the guidance of ultrasound and within a meticulously controlled sterile environment. The instrument is accurately positioned at the location predetermined by physicians to achieve desired outcomes.
Furthermore, brachytherapy at FV is guided by advanced 3D simulation techniques, enabling doctors to have a clear view of internal organs and simulate interactions between radiation beams and organs to optimise dose distribution. FV is also capable of performing interstitial brachytherapy (simulated using MRI) for cases with irregularly shaped tumours, allowing for a comprehensive dose distribution throughout the entire tumour.

Dr Basma M’Barek advises a patient on cancer treatment.
Leveraging its strength as a multi-specialty hospital, FV Hospital ensures patients undergo interdisciplinary tumour board consultations involving experts in oncology, imaging diagnostics, and various surgical specialties. These doctors contribute their insights and collectively reach a consensus on every individualised treatment protocol, developed specifically for every patient.
To learn more about cancer treatment at FV Hospital, please call: (028) 54 11 33 33.



