In capsule endoscopy, the patient swallows a compact capsule that enables doctors to see inside the gastrointestinal tract non-invasively. It also provides visuals of the deep part of the small intestine, often considered the “blind spot” of other popular endoscopic techniques.
Detection and treatment of small bowel pathology by capsule endoscopy
Patient Trinh Van H. (44 years old, residing in HCMC) was hospitalised at the Gastroenterology & Hepatology Department, FV Hospital, on March 2, 2022, with black stools, anaemia, and a dull pain that he’d been experiencing around his navel area for the previous month. His gastroscopy and colonoscopy results showed that Mr H. had mild gastritis and diverticulitis of the entire colon, but there was no sign of bleeding.

Patient undergoes gastrointestinal endoscopy at FV Hospital
After two days in hospital, a mass of fresh blood was discovered in Mr H.’s stool and his Hgb index (haemoglobin index in the blood) was only 6.5 grams per decilitre—half that of a healthy adult. Mr H. received an urgent blood transfusion and was assigned capsule endoscopy. In addition to the problems detected previously, the image showed that the patient had erosive ulcerative colitis in the middle section of his small intestine and small polyps in the rectum.
FV Hospital’s doctors adjusted his medical prescription after discovering the cause of bleeding. Two days after capsule endoscopy, patient H.’s condition rapidly improved and he no longer had black or bloody stools and his Hgb index stabilised. Mr H. was discharged on 8 March 2022.
FV Hospital’s treated a similar case later that year. In September 2022, patient David M. (65 years old, British nationality) was admitted to the hospital after many days with symptoms of black stools and anaemia with an Hgb index of only 6.4 g/dL. Despite active blood transfusion, his condition did not stabilise.
Suspecting that the patient had hidden gastrointestinal bleeding, doctors ordered a gastroscopy, but only mild inflammation was detected. They did not perform a colonoscopy due to Mr M.’s cardiovascular contraindications, but instead assigned him to participate in capsule endoscopy which yielded key insights: he had diffuse congestive inflammation throughout the stomach, small intestine, and colon—doctors observed red inflamed areas with signs of bleeding and multiple ulcers in the ileocecal segment of his gut (the junction between the colon and the small intestine). Doctors quickly treated Mr M. and his stools and Hgb index gradually returned to normal.
Capsule endoscopy opens a new chapter in the treatment of small bowel diseases
Dr Bui Nhuan Quy, Specialisation Level II, Head of Gastroenterology & Hepatology Department, FV Hospital, said that bleeding, ulcers, malabsorption, stenosis, polyps, cancer, and other diseases related to the small intestine are not particularly common but cases are rising. One study showed that in 911 cases of occult gastrointestinal bleeding (haemolysis in the stool), capsule endoscopy enabled doctors to find the cause in 509 cases (56%). Of those 509 cases, one-fifth were caused by diseases related to the small intestine.
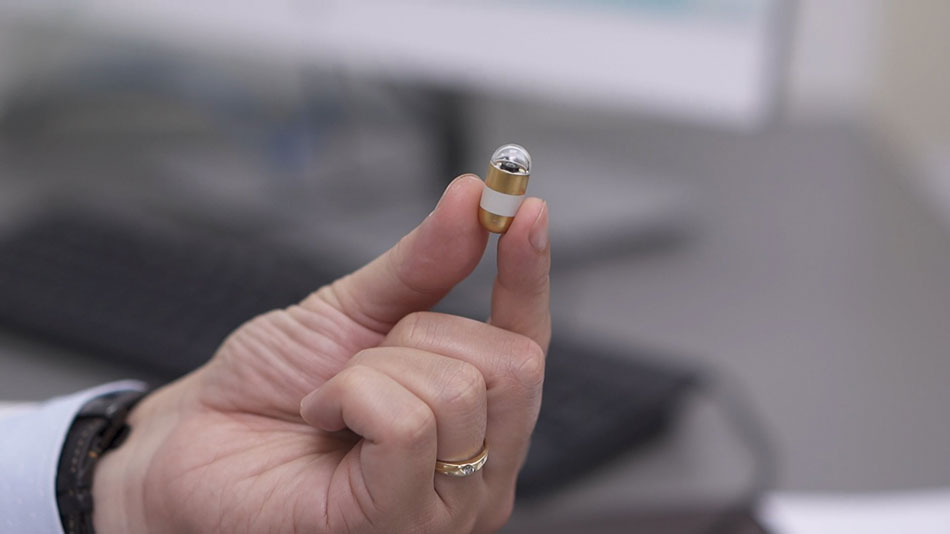
A capsule endoscopy device – the same size as an oral medication capsule
General endoscopy procedures, including upper gastrointestinal endoscopy (gastroscopy), colonoscopy, and small bowel endoscopy (including push, single, double, and spiral), are not able to examine the whole small intestine. Furthermore, these techniques require general anaesthesia, long execution times, complex techniques, and use of X-rays that expose the patient to radiation.
The small intestine is considered a “blind spot” for most imaging techniques, so in the past, diseases related to the small intestine were often detected only in the advanced stage of the disease, such as when a large tumour began causing massive gastrointestinal bleeding or intestinal obstruction, or a tumour ruptured, causing peritonitis.

Dr Bui Nhuan Quy explains the advantages of capsule endoscopy
“The precise detection of the location of bleeding plays a huge role in the correct treatment. Minimal intervention is required to help restore the patient’s health before potentially life-threatening issues occur,” says Dr Quy.
Capsule endoscopy was first deployed in 1981 to give gastroenterologists a better view of the inside of the small intestine. The compact unit consists of a capsule camera, light source, battery and transmitter.
When swallowed, the device moves through the gut with the body’s natural peristaltic motion and transmits images obtained throughout to a wireless receiver worn by the patient at their waist. After 11 to 12 hours, the receiver will automatically disconnect, and the capsule will be expelled from the body through excretion. Each camera capsule is designed for single use by one patient.
Capsule endoscopy makes it possible to visually observe areas of the gastrointestinal tract that are inaccessible to optical endoscopes, and it has many other advantages: it’s non-invasive, is not time-consuming for patients to undergo, and does not require that the bowel be prepared for the procedure, for instance by fasting and flushing out stool, a required process prior to colonoscopy. This method does not require the patient to stop taking important drugs, does not need sedation or pain medication, and is not limited to patients with cardiopulmonary disease and dangerous complications such as bleeding or damage to the intestinal lining.
This technique is often indicated by doctors to detect small bowel pathologies, such as finding the cause of hidden gastrointestinal bleeding, investigating anaemia originating from the gastrointestinal tract when upper and lower endoscopy has not revealed the cause, in the detection of Crohn’s disease and Celiac disease, and assessing mucosal healing and polyposis syndrome.
Capsule endoscopy technique gives impactful results in the first 24 hours
Capsule endoscopy appeared in Vietnam 10 years ago, but was expensive: each wireless receiver cost VND 400 million and capsules cost VND 12 to 13 million each. Diseases related to the small intestine were much less common compared to the diseases of the colon and stomach, so most hospitals continued to use typical endoscopic equipment and rented equipment when capsule endoscopy was indicated, which usually took round two or three days.

A patient at FV Hospital swallows an endoscopic capsule
Time is an extremely important factor. Clinical practice shows that capsule endoscopy can detect up to 55 per cent of bleeding locations if the patient develops bleeding in the first 24 hours. If detection is delayed by five days, the detection rate is only 18 per cent.
FV Hospital is one of the few medical facilities that has a capsule endoscope system available for patients, making examination and diagnosis more convenient in one location. FV Hospital’s Gastroenterology & Hepatology Department team monitors and guides patients when taking capsules and can answer any question patients might have regarding wearing the wireless receiver at home. When the recording time is completed, FV staff will visit the patient’s residence to collect the equipment and return it to doctors so that the team can review results and give specific treatment directions.
Being equipped for capsule endoscopy helps doctors to provide timely diagnosis and appropriate treatment for hospitalised patients. In emergency cases when a patient is experiencing a serious degree of internal bleeding, waiting for third party device rental support can outstrip the “golden” time period for bleeding location detection.
“In the case of patient David M., who had severe gastrointestinal bleeding and a history of cardiovascular disease, without capsule endoscopy we would have to hope the wound would stop bleeding on its own and the patient’s body would heal naturally.
“If the bleeding had continued, the patient may have needed to undergo exploratory surgery, when we would make a small incisions on the abdomen to insert the laparoscopic device into each segment of the patient’s small intestine, all of which would need suturing afterwards. This invasive method must be performed under sedation in the operating room, which is more risky for the patient, and increases likelihood of serious health sequelae after surgery,” says Dr Quy.
To book an appointment at the Gastroenterology & Hepatology Department, FV Hospital, please contact: (028) 54 11 33 33.



