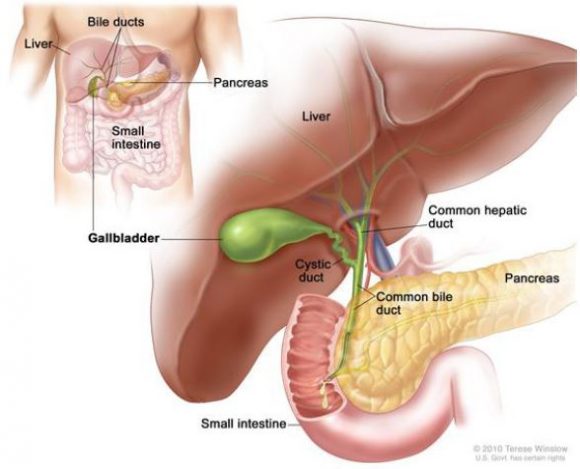
WHAT IS THE GALLBLADDER?
The gallbladder is a small, pear-shaped pouch that lies under the liver in the upper-right part of your abdomen. It stores and concentrates bile, a digestive liquid continually secreted by the liver. The bile emulsifies fats and neutralizes acids in partly digested food.
WHEN IS CHOLECYSTECTOMY INDICATED?
A cholecystectomy is an operation to remove the gallbladder.
- Cholecystectomy is usually indicated in patients with presence of gallstones. Gallstones often cause no symptoms and in many cases remain undetected but they can cause blockage of the gallbladder, inflammation and infection. Symptoms of gallbladder disease include pain, vomiting, nausea, fever and sometimes jaundice.
- GB polyps: cholecystectomy is also indicated in patients with gallbladder polyps greater than 10 mm or unequivocal recurrent biliary colic, especially in case of coexistence of stones and polyps.
- GB cancer: Gallbladder cancer may be treated with a surgery to remove the gallbladder and some of the tissue around it. Nearby lymph nodes may also be removed.
TYPES OF CHOLECYSTECTOMY
There are two ways of performing a cholecystectomy:
Laparoscopic cholecystectomy
This is the most common way of having your gallbladder removed. The operation is carried out using a camera and surgical instruments that are inserted through small incisions (cuts) in your abdomen.
Laparoscopic cholecystectomy does not require the abdominal muscles to be cut, resulting in minimal post-operative pain, quicker healing, improved cosmetic results, and fewer complications such as infection and adhesions.
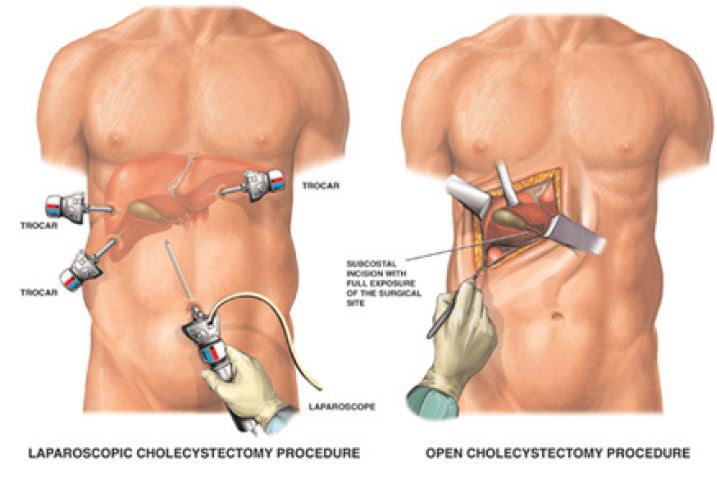
Open cholecystectomy
The gallbladder is removed through one large cut in your abdomen. This technique is called
open surgery. It is a more invasive operation than keyhole surgery, you need to be in hospital
for longer and it takes longer to recover. Open surgery is rare in modern practice.
Cholecystectomies (laparoscopic and open) are performed under general anesthesia (you are
asleep during it).
There is 1 to 5% chance of conversion from laparoscopy to open surgery. Factors that may increase the possibility of choosing or converting to the “open” procedure may include obesity, a history of prior abdominal surgery causing dense scar tissue, inability to visualize organs or bleeding problems during the operation or in emergency When the surgeon feels that it is safest to convert the laparoscopic procedure to an open one, this is not a complication, but rather sound surgical judgment.
PREPARATION BEFORE OPERATION
You will need to attend a pre-anesthesia appointment a few days before surgery. The appointment may involve having some blood tests and a general health check depending on your age and medical condition to make sure that you are fit for surgery.
It is recommended that you shower with Betadine scrub the night before and morning of the operation.
After midnight the night before the operation, you should not eat or drink anything except medications that your surgeon or Anesthetist has told you are permissible to take with a sip of water the morning of surgery.
COMPLICATIONS OF CHOLECYSTECTOMY
While there are risks associated with any kind of operation, the vast majority of laparoscopic gallbladder patients experiences few or no complications and quickly return to normal activities.
Complications of laparoscopic cholecystectomy are infrequent, but include bleeding, infection, pneumonia, blood clots, or heart problems. Unintended injury to adjacent structures such as the common bile duct or small bowel may occur and may require a conversion into open surgery or another surgical procedure to repair it. Bile leakage into the abdomen from the tubular channels leading from the liver to the intestine may rarely occur.
RECOVERY AFTER SURGERY
Once liquids or a diet is tolerated, patients leave the hospital the same day or few days following the laparoscopic gallbladder surgery.
Activity is dependent on how the patient feels. Walking is encouraged.
The onset of fever, yellow skin or eyes, worsening abdominal pain, distention, persistent nausea or vomiting, or drainage from the incision are indications that a complication may have occurred. Your surgeon should be contacted in these instances.
Most patients can return to work within seven days following the laparoscopic procedure depending on the nature of your job. Patients with administrative or desk jobs usually return in a few days while those involved in manual labor or heavy lifting may require a bit more time. Patients undergoing the open procedure usually resume normal activities in four to six weeks.
SO WHAT HAPPENS AFTER YOUR DISCHARGE?
Well, sometimes you may have some problem for fat digestion. But luckily, since your body is so amazing, your liver will take over some of the gallbladder’s job. So after some weeks you will be able to eat normally many times better than before the surgery.



