COLONOSCOPY OVERVIEW
Colonoscopy is an investigation that allows your doctor to look at the inner lining of your large intestine (rectum and colon) using a thin, flexible tube called a colonoscope. A colonoscopy helps find ulcers, polyps, tumors, and areas of inflammation or bleeding. During a colonoscopy, tissue samples can be collected (biopsy) and abnormal growths can be taken out. Colonoscopy can also be used as a screening test to check for cancer or precancerous growths (polyps).
Colonoscopy is carried out in hospital and is usually done as a day case. This means you have the test and go home the same day. The procedure itself usually takes about 30 to 45 minutes. The colonoscope is a thin, flexible tube that ranges from 122 cm to 183 cm long, approximately the size of an index finger.

A small video camera is attached to the colonoscope so that your doctor can take pictures or video of the large intestine. The colonoscope can be used to look at the whole colon and the lower part of the small intestine. The test called sigmoidoscopy shows only the rectum and the lower part of the colon.
INDICATIONS FOR COLONOSCOPY
- Abdominal pain, changes in bowel movements, chronic diarrhea, or weight loss
- Abnormal changes (such as polyps) found on sigmoidoscopy or x-ray tests (CT scan or barium enema)
- Anemia due to low iron
- Blood in the stool, or black, tarry stools
- Follow-up of a past finding, such as polyps or colon cancer
- Inflammatory bowel disease (ulcerative colitis and Crohn’s disease)
- Screening for colorectal cancer
- Colonoscopy is recommended by the American Cancer Society (ACS), the American College of Gastroenterologists (ACG), the American Gastroenterological Association (AGA), and the U.S. Preventive Services Task Force (USPSTF)
- These groups recommend routine testing for people age 50 and older who have a normal risk for colorectal cancer.
- Your doctor may recommend earlier or more frequent testing if you have a higher risk for colorectal cancer. Talk to your doctor about when you should be tested.
- As an alternative to colonoscopy, your doctor may also propose you to undergo a virtual colonoscopy (also called a large bowel CT scan).
MEDICATIONS – INFORMED CONSENT
Before you have a colonoscopy, tell your doctor if you:
- Are taking any medicines, such as insulin or medicines for arthritis (check with your doctor about which medicines you can or cannot take on the day of your test).
- Are allergic to any medicines, including anesthetics.
- Have bleeding problems or take aspirin or other blood thinners such as warfarin/ Sintrom®, Coumadin® , clopidogrel/Plavix®.,
- Had an X-ray test using barium, such as a barium enema, in the last 4 days.
- Are or might be pregnant.
You may be asked to stop taking aspirin products or iron supplements 7 to 14 days before the test. If you take blood-thinning medicines regularly, discuss with your doctor how to manage your medicine.
You will be asked to sign a consent form that says you understand the risks of colonoscopy and agree to have the test done. Talk to your doctor about any concerns you have regarding the need for the test, its risks, how it will be done, or what the results will mean.
Because colonoscopy is done under general aneasthesia you will need to have a consultation with the aneasthesiologist usually 48 hours before the test, the anaesthesiologist may require some blood testing

PREPARATION
Before the colonoscopy, your colon must be cleaned out. The following information gives you a general idea of the preparation for a colonoscopy. Your doctor will give you specific instructions before your test.
- One to two days before the test, you will stop eating solid foods and drink only clear fluids, such as water, tea, coffee, clear juices, clear broths. Do not drink anything red or purple, such as grape juice or wine
- Your doctor will prescribe you a laxative mixed with water that you will be asked to drink over 1 to 2 hours. You will begin to have watery diarrhea within a short time after drinking the laxative solution. This solution may taste very salty and may make you feel sick to your stomach. To make your colon prep easier, you may want to try some of the following tips:
- Each time you drink some of the solution, you may also drink some water or clear fluids (like apple juice) to help get rid of the salty taste in your mouth.
- You may find it easier to drink the solution if you chill it in the refrigerator first.
- Add lemon juice to the solution or suck on sliced lemon wedges after you take a drink.
- You will want to stay home the evening before the test because the colon prep will make you use the bathroom often.
- Drink plenty of clear fluids during the prep so you will not get dehydrated. This will also help clean out your colon completely after you finish the colon prep.
- Do not eat any solid foods after drinking the laxative solution.
- Stop drinking clear liquids 6 to 8 hours before the colonoscopy.
- Your doctor may have you use an enema 30 to 60 minutes before the test to completely clean out your colon.
Arrange to have someone take you home after the test because you may be given a medicine (sedative) to help you relax before the test and you will not be able to drive safely.
WHAT TO EXPECT ON THE DAY OF COLONOSCOPY
Patients are admitted in the Day Hospitalisation Ward and the colonoscopy then performed in the dedicated, well-equipped, endoscopy unit in the operating theatre.
During the test, you may get a pain medicine and a sedative put in a vein in your arm (IV). These medicines help you relax and feel sleepy during the test. You may not remember much about the test.
You will need to take off most of your clothes. You will be given a gown to wear during the test.
You may lie on your left side with your knees pulled up to your belly. The doctor will gently put a gloved finger into your anus to check for blockage. Then he or she will put the thin, flexible colonoscope in your anus and move it slowly through your colon. The doctor can look at the lining of the colon through the scope or on a computer screen hooked to the scope.
You may feel the need to have a bowel movement while the scope is in your colon. You may also feel some cramping. Breathe deeply and slowly through your mouth to relax your belly muscles. This should help the cramping. You will likely feel and hear some air escape around the scope. There is no need to be embarrassed about it. The passing of air is expected. You may be asked to change your position during the test.
Your doctor will look at the whole length of your colon as the scope is gently moved in and then out of your colon.
The doctor may also use tiny tools, such as forceps, loops, or swabs, through the scope to collect tissue samples (biopsy) or take out growths. Usually, people do not feel anything if a biopsy is done or if polyps are taken out.
The scope is slowly pulled out of your anus and the air escapes. Your anal area will be cleaned with tissues. If you are having cramps, passing gas may help relieve them.
The test usually takes 30 to 45 minutes, but it may take longer, depending upon what is found and what is done during the test.
After the test, you will be watched for 1 to 2 hours. When you are fully awake, you can go home. You will not be able to drive or operate machinery for 12 hours after the test. Your doctor will tell you when you can eat your normal diet (most people are able to eat normally after the test) and do your normal activities. Drink a lot of fluid after the test to replace the fluids you may have lost during the colon prep but do not drink alcohol. Ask your doctor when it is safe to restart aspirin and other blood-thinning medications if you usually take these medications.
After the test, you may have bloating or crampy gas pains and may need to pass some gas. If a biopsy was done or a polyp taken out, you may have traces of blood in your stool (feces) for a few days. If polyps were taken out, your doctor may instruct you to not take aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs) for 7 to 14 days.
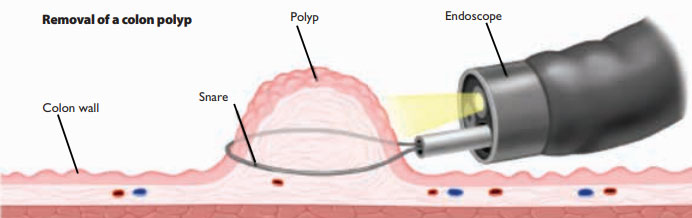
COLON POLYP REMOVAL
Procedure — Polyps are usually removed when they are found on colonoscopy, which eliminates the chance for that polyp to become cancerous. The medical term for removing polyps is polypectomy. Small polyps can be removed with an instrument that is inserted through the colonoscope and snips off small pieces of tissue. Larger polyps are usually removed by placing a noose, or snare, around the polyp base and burning through it with electric cautery. The cautery also helps to stop bleeding after the polyp is removed.
Polyp removal is not painful because the lining of the colon does not have the ability to feel pain. In addition, a sedative medication is given before the colonoscopy to prevent pain caused by stretching of the colon. Rarely, a polyp will be too large to remove during colonoscopy, which means that a surgical procedure will be needed at a later time.
One way doctors remove colon polyps is to use a noose as a tool. They loop a wire around the polyp and squeeze the loop tight. When the polyp comes off, the doctor sucks it up into the endoscope, so that it can go to the lab for tests.
After polyp removal — Medications that can increase bleeding, including aspirin, ibuprofen (Advil®, Ibudolor®, Motrin®), and naproxen (Aleve®), should be avoided for approximately two weeks after polypectomy. Acetaminophen (Tylenol®) is safe to take. People who require anticoagulant medications such as warfarin (Sintrom®, Coumadin®) must discuss how and when to resume this medication with their clinician.
COLONOSCOPY COMPLICATIONS
Colonoscopy is a safe procedure, and complications are rare but can occur:
- The colonoscope can cause a tear or hole in the colon. This is a serious problem, but it does not happen commonly.
- Bleeding can occur from biopsies or the removal of polyps, but it is usually minimal and can be controlled.
- Reactions to the anaesthetics are possible
Polypectomy is safe although it has a few potential risks and complications. The most common complications are bleeding and perforation (creating a hole in the colon). Fortunately, this occurs infrequently (one in 1000 patients having colonoscopy). Bleeding can usually be controlled during colonoscopy by cauterizing (applying heat) to the bleeding site; surgery is sometimes required for perforation.
After the test, call your doctor immediately if you:
- Have rectal bleeding.
- Have severe belly pain (not just gas cramps)
- Develop a fever.
- Are very dizzy.
- Are vomiting.
- Have a swollen and firm belly.
RESULTS OF THE PROCEDURE
Your doctor can describe the results of the colonoscopy as soon as it is over.
If a sample of tissue (biopsy, polypectomy) was collected during the colonoscopy, it will be sent to a lab for tests:
Samples of colon tissue are usually sent to a pathology lab, where they are looked at under a microscope for diseases.
Other samples of colon tissue may be sent to a microbiology lab to see whether an infection is present.
The results of tests sent to a lab will be available within one to two weeks
A follow-up appointment or phone call is usually scheduled after polyp removal or biopsy to discuss the results of the tissue analysis.



