WHAT IS PERCUTANEOUS ABSCESS DRAINAGE?
An abscess is an infected collection of fluid in the body. In general, people who have an abscess will experience fever, chills and pain. Once the diagnosis of an abscess has been made, after an ultrasound or CT scan, an assessment is made, by your doctor and an interventional radiologist, to decide to perform a percutaneous drainage (or a puncture for liquid sampling and analyse) to help abscess treatment.
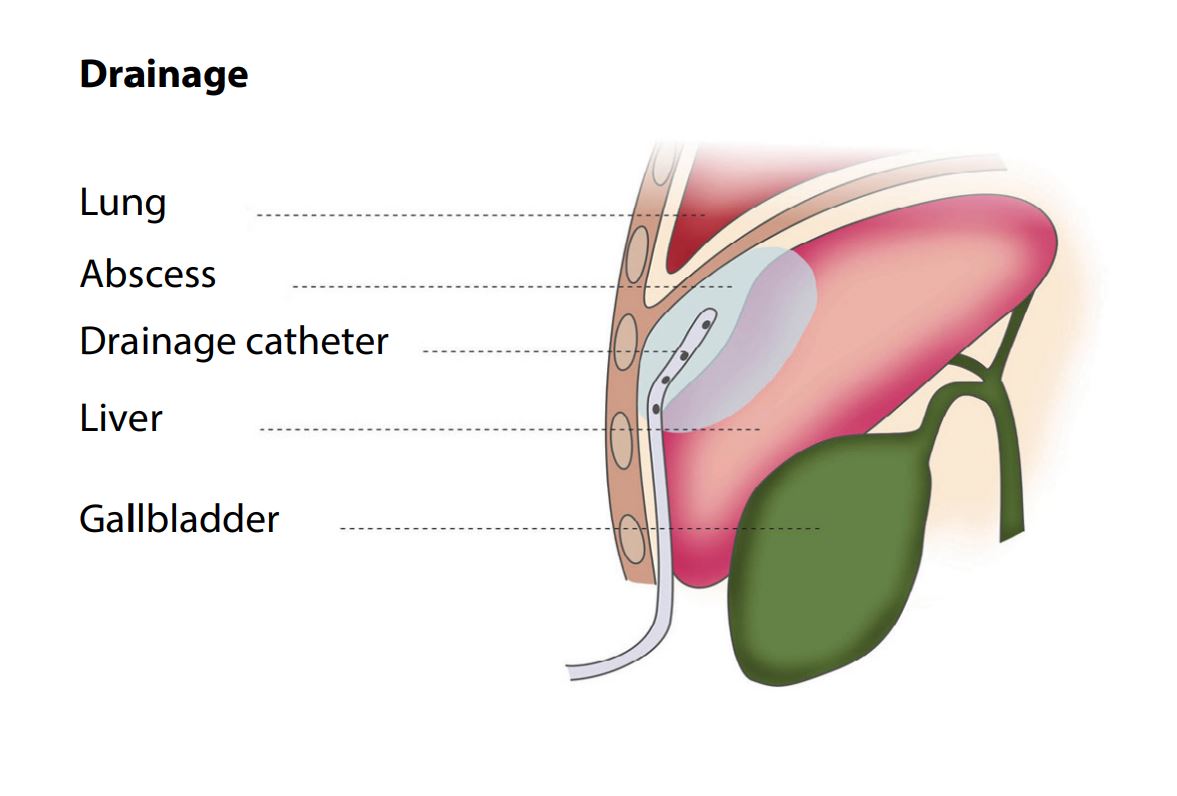
In percutaneous abscess drainage, doctors use imaging guidance to place a thin needle to remove or drain infected fluid (abscess) from the body. Usually, a drainage tube is left in place a few days to avoid recurrence. Occasionally, depending on the location, abscesses that cannot be cured by percutaneous drainage may require more extensive surgical drainage in the operating room.
WHAT ARE SOME COMMON USES OF THE PROCEDURE?
Percutaneous abscess drainage is generally used to remove infected fluid from the body, most commonly in the abdomen and pelvis. The abscess may be a result of recent surgery or secondary to an infection such as diverticulitis. Less commonly, percutaneous abscess drainage may be used in the chest or elsewhere in the body.
HOW SHOULD I PREPARE?
Patients who undergo percutaneous abscess drainage fall into two general categories:
- those who are hospitalized, frequently recovering from surgery.
- those who are not hospitalized and have symptoms as described above. In these cases, you may be admitted to the hospital on the day of your procedure.
You should report to your doctor all medications that you are taking and if you have any allergies, especially to local anaesthetic medications, general anaesthesia or to contrast materials. Your doctor may advise you to stop taking aspirin, non-steroidal anti-inflammatory drugs or a blood thinner for a specified period of time before your procedure.
You will be asked to fill out a Questionnaire and a Consent form prior to the exam.
Women should always inform their doctor or the diagnostic radiographer if there is any possibility that they are pregnant. Many imaging tests are not performed during pregnancy so as not to expose the foetus to radiation. If an x-ray is necessary, precautions will be taken to minimize radiation exposure to the baby.
You may be instructed not eat or drink anything for several hours before your procedure.
You will be given a gown to wear during the procedure.
You should plan to stay at the hospital following your procedure.
HOW IS THE PROCEDURE PERFORMED?
Image-guided, minimally invasive procedures such as percutaneous abscess drainage are most often performed by a specially trained interventional radiologist under CT scanner or Ultrasound guidance.
You will be positioned on the examining table.
Your doctor will numb the area with a local anesthetic.
The area of your body where the catheter is to be inserted will be sterilized and covered with a sterile surgical drape.
A very small nick is made in the skin at the site.
Using image-guidance, a catheter (a long, thin, hollow plastic tube) is inserted through the skin and manipulated to the site of the abscess to allow drainage of the infected fluid.
This procedure is usually completed in 20 minutes to an hour.
If needed, the catheter, fixed to the skin by some sutures, may be connected to a drainage bag outside of your body. The tube will remain in place until the fluid has stopped draining and your infection is gone. It may take several days to drain the abscess.
Samples of fluid may be collected for analysis.
WHAT WILL I EXPERIENCE DURING AND AFTER THE PROCEDURE?
You will feel a slight pin prick when the needle is inserted into your vein for the intravenous line and when the local anesthetic is injected.
You may feel slight pressure when the catheter is inserted but no serious discomfort.
In general, patients who undergo percutaneous abscess drainage will remain hospitalized for a few days. Further follow up is usually done on an outpatient basis and you will be seen by your doctor at regular intervals to ensure that the healing process is proceeding according to plan. Once you have recovered and your doctor is satisfied that healing is complete, the catheter will be removed.
WHO INTERPRETS THE RESULTS AND HOW DO I GET THEM?
The interventional radiologist can advise you as to whether the procedure was a technical success when it is completed.
In case of sampling, a pathologist examines the collected specimen and makes diagnosis.
WHAT ARE THE BENEFITS VS. RISKS?
Benefits
- No surgical incision is needed—only a small nick in the skin that does not have to be stitched closed.
- The procedure is minimally invasive and the recovery period is usually faster than after open surgical drainage.
Risks
- Any procedure where the skin is penetrated carries a risk of infection. The chance of infection requiring antibiotic treatment appears to be less than one in 1,000.
- There is a very slight risk of an allergic reaction if contrast material is injected.
- Very rarely, an adjacent organ may be damaged by percutaneous abscess drainage.
- Occasionally bleeding may occur. This can typically be treated by minimally invasive techniques, if necessary.
- The catheter placed at the time of percutaneous abscess drainage may become blocked or displaced requiring manipulation or changing of the catheter. In addition, a very large or complex fluid collection may require more than one abscess drain.
How do I schedule a Percutaneous Abscess Drainage?
For further information and for taking appointment, kindly contact our imaging department at (08) 54 11 34 00



