Head and neck cancer is the term used to describe a number of different malignant tumours that develop in or around the throat, larynx, nose, sinuses, salivary glands and mouth. Their treatment can include surgery, chemotherapy or radiotherapy, either alone or in combination.
WHAT IS RADIOTHERAPY?
Radiotherapy is the use of high energy X-rays (radiations) to treat cancer. Radiotherapy works by causing damage to the cancer cells in the treatment area. Although some normal healthy cells are affected, these are able to recover and repair themselves.
It is delivered using a machine called a linear accelerator. Radiotherapy does not hurt, the machine does not touch you and it is very much like having an ordinary X-ray.
There are several types of radiotherapy. Head and neck cancers are better treated using Intensity-Modulated RadioTherapy (IMRT) or Volumetric Modulated Arc Therapy (VMAT) techniques which are both available at Hy Vong Cancer Centre.
Radiotherapy is given as outpatient treatment. Treatment is given over a prescribed number of days/weeks so that only small doses of radiation are given at each session. A typical course of radiotherapy for the head and neck lasts between 3 to 7 weeks and each radiotherapy session will take between 15-20 minutes to position and deliver.
Radiotherapy does not make you radioactive and you are safe to be around others (including children and pregnant women) throughout your sessions.

WHAT HAPPENS BEFORE RADIOTHERAPY STARTS?
Dental assessment
You need to see the dentist before you start your radiotherapy. This is to check for any decaying or “at risk” teeth that may need to be removed. You may also require a “gutter” to be made for you. This is placed in your mouth during treatment to apply fluorine on your teeth to avoid tooth decay.
Please read the FV Hospital brochure “Dental Protection and Radiotherapy”.
Dietician review
It is important to involve a dietician/medical nutritionist before, during and after treatment to help you prevent further weight loss and/or cancer cachexia. A dietician/medical nutritionist will also provide you nutrition advice when necessary and monitor your nutritional status throughout the treatment.
Pregnancy
If you are a woman of childbearing age you should not become pregnant before or during radiotherapy because the treatment may harm the baby you are carrying, especially in the first three months of a pregnancy. If necessary, please speak to your doctor about contraception methods suitable for use during radiotherapy.
Pacemakers
If you have a pacemaker, please tell your doctor as soon as possible. You will need to have your pacemaker checked before your radiotherapy treatment.
Drinking and Smoking
You are advised to stop smoking during treatment as it will make any soreness in your throat worse and may delay the healing process that could make the treatment less effective. Support and advice can be given on quitting smoking, you can take an appointment with the Quit Smoking Clinic of FV Hospital.
Drinking alcohol will irritate the lining of the mouth and throat and is not recommended during treatment.
HOW IS THE TREATMENT PLANNED?
Plastic mask
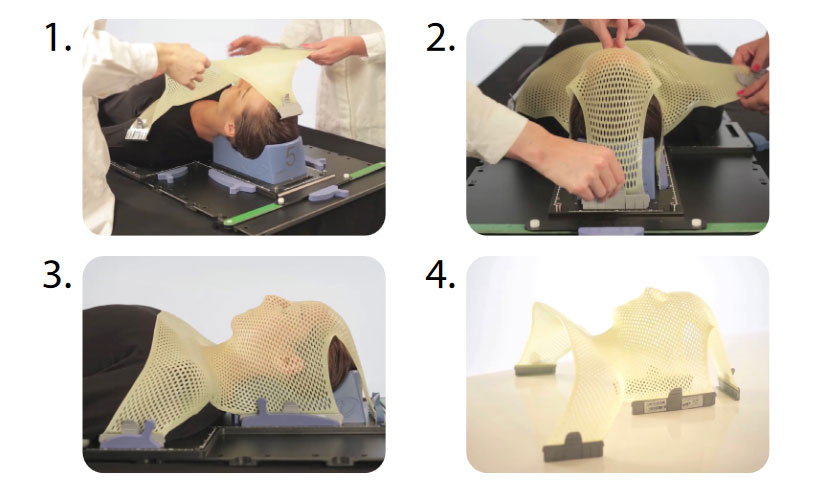
We will make you a plastic mask that will hold your head and neck in exact same position for each session. The mask is designed so that you can breathe normally while wearing it.
To make the mask, a thin sheet of plastic will be warmed in a special oven to make it softer. This is then placed over your face and moulded to the bridge of the nose and chin. The mask will become rigid as it dries and may feel a little tight. This is normal and will help to keep your head still. The mask-making process takes around 10 minutes but your appointment may last 30 minutes in total.
The mask needs to be a very snug fit. We need facial hair (beards and moustaches) trimmed very short or for you to be clean shaven before attending the mask appointment.
It may happen that the mask does not fit you well enough at one point during treatment; it might be because you have lost weight or for other reason, in that case the mask will have to be recast or a new one made.
The following images show how the mask is made:
Your oncologist may request a mouth bite for you to wear inside the mouth during the planning CT scan and your sessions. The mouth bite separates the top and bottom of the mouth to help reduce pain during treatment.

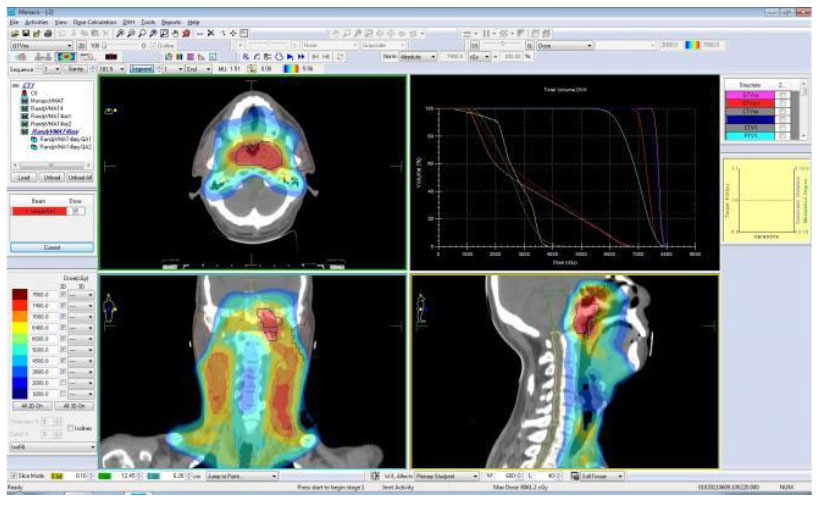
CT scanner
You will have a CT scan while wearing the new mask. It is often necessary to have a contrast injection to provide clearer CT images. The images will be used to reconstruct a three dimensional image of your head and neck. Your oncologist will then use this image to plan exactly where you will be treated with radiotherapy.
It may happen that a second CT scan is deemed necessary during treatment, for example if the tumour size has quickly reduced. This is required to accurately adjust your radiotherapy.
WHAT WILL HAPPEN DURING THE TREATMENT?
At each treatment session, you will be asked to change in a cubicle, and then a radiographer will take you into the treatment room. You will lie on the treatment table, and your mask will be placed over your face. The radiographer will move the treatment table to make sure you are in the right position. When they are satisfied with the position, they will leave the room.
X-ray images are taken regularly during your treatment to make sure that the treatment is being delivered accurately. There will be a short delay while these images are assessed and you may feel the bed move as the radiographers adjust your position from outside of the room.
Treatment will then be delivered and the machine will move around you to treat you from different angles. You will not feel anything but you may hear a bleeping sound. During the treatment, you will be alone in the room but the radiographer will watch you all the times on a monitor. If you need assistance, you can raise your hand and the radiographer will come back into the room.
When you are positioned correctly, the treatment table will be quite high up, so it is very important that you do not move or try to get off the table without help.
After the treatment is complete, the radiographer will return to the room, remove the mask and help you down from the treatment table. The radiographer will tell you when it is safe to sit up and get off the table.
Each radiotherapy session can take between 15-20 minutes to position and deliver.
Please inform any of your medical team as soon as possible if you notice any change in yourself or your normal routine, such as a change in diet, weight, sleeping habits, increased discomfort or pain.
The side effects of radiotherapy to the head, neck and chest region may be aggravated by alcohol consumption and cigarette smoking, Therefore all patients are advised to stop smoking and minimise their alcohol intake. This is especially important during and immediately after treatment.
WHAT SIDE EFFECTS CAN I EXPECT?
You may begin to notice some side effects during your second or third week of radiotherapy. It’s important to remember that treatment reactions are very individual and the severity will differ from person to person.
You will be seen regularly by your oncologist and your dietician to review how you are managing and ensure you have plenty of support to help you complete the course of treatment. You may need to be seen by a speech therapist to help if you have swallowing problems.
Tiredness
You are likely to feel more tired during your radiotherapy, especially towards the end of the treatment sessions. It may help if you can plan your day so you have time to rest and do things that are important to you when you feel least tired. Try to get enough sleep.
You may need support to help with your everyday activities such as shopping, laundry and meal preparation.
Soreness of the mouth and the throat
At first you may notice that your mouth becomes drier. As the treatment progresses, areas of the mouth may ulcerate and become swollen and sore. You may also produce sticky mucous. Your throat may become sore inside making it difficult to swallow. Medications can be prescribed to control pain and help make swallowing easier.
It is important during the treatment to drink plenty of fluids and keep your mouth healthy. Good oral hygiene includes gently brushing your mouth and tongue using a soft toothbrush, flossing daily and using a mouthwash regularly. Your healthcare team will provide you with advice regarding the appropriate mouth care. They will advise you on how to prepare and use mouthwashes.
Please read the FV Hospital brochure “Mouth Sores and Cancer Treatment”.
Dryness of the mouth
Your salivary glands may be affected by the radiotherapy treatment. Saliva lubricates the mouth, protects the teeth and starts the process of digestion. This dryness may last for quite a few months and in some cases may be permanent.
Taste changes
Taste changes or even loss of taste can be caused directly by the radiotherapy or indirectly by the dry and sore mouth. You may find that food taste bland or you may not taste anything. This can last up to 8 weeks after you finish your treatment.
Eating problems
Drink plenty of fluids. Drink enough water with your meals to make it easier to swallow food. Sip cold drinks such as non-acid fruit juice or aromatic plants infusions (camomile) in between your meals. Use a straw if your mouth is sore. Try to drink six large glasses of fluids per day especially before, during and after treatment.
Try eating smaller, more frequent meals. Avoid sour, salty or acidic fruits and juices such as orange, grapefruit and tomatoes. Avoid spices and spicy foods that may irritate the mouth. Limit rough, coarse or dry foods with sharp edges, such as raw vegetables, potato chips, pretzels or nuts. Use a blender to soften or puree foods if chewing or swallowing becomes difficult.
Eat soft, moist, bland foods that are lukewarm or cool in temperature. Hot foods or fluids (coffee, tea) can irritate a sore mouth. Ice cream or sugar-free popsicles provide needed fluids and help comfort inflamed areas. Sucking on these just before and during treatment may be helpful.
Feeding tubes or Percutaneous Endoscopic Gastrostomy (PEG) feeding methods, to deliver nutrition directly to the stomach, are sometimes necessary.
Loss of appetite and weight loss:
- Try to make the most of when your appetite is good – have regular meals and snacks;
- Try different foods, you may find you like things you would not usually eat;
- Do not try to eat large meals. Try eating small amounts more often. Aim for 6 small meals and nourishing snacks each day between meals;
- Make food as nourishing as possible. If you cannot tolerate solid foods, try a nourishing drink e.g. milk, creamy soup, pureed, jellified drinks, custard, yogurt and Oral Nutritional Supplement
- Aim to have good source of protein with meals and snacks.
- Let people cook for you. Cooking your own food can be tiresome and off-putting. Convenience foods can be useful standbys;
- Try to relax and enjoy what you eat. A short walk before a meal or simply getting some fresh air may help you give you an appetite.
Making the most of your food:
- Enriching your food with nutrients and extra calories is important to help maintain your weight;
- Use full fat dairy products, especially milk and yoghurts, instead of the low fat types;
- Add dried milk powder to soups, sauces, milky puddings and custards;
- Add cheese and cream to food such as mashed potatoes, creamy sauces and soup;
- Use extra spreads or dressings such as full-fat butter, margarine, mayonnaise, peanuts butter, chocolate spread, jam or marmalade;
- Add white or brown sugar, honey, syrup or treacle to cereals, drinks or desserts;
- Try adding extra gravy, butter or margarine to increase moisture to your food.
Vocal changes
If your larynx is included in the treatment area you may find that your voice becomes hoarse and croaky over the course of your treatment. Although this will continue in the weeks after treatment it should improve over time.
Your speech and language therapist and other members of the healthcare team will provide you with information and advice to help you take care of your voice.
Skin soreness
The skin in the treated area will gradually become dry and slightly reddened, very much like sunburn. It can even peel or weep. The severity of the reaction varies from person to person and there are a variety of different creams, gels and dressings that are available if required.
Wash your skin using non-perfumed soap. The area should be washed gently with lukewarm water and patted dry with a soft clean towel.
Do not expose your skin to the sun during treatment, if you go out in the sun, use a suncream that is rated SPF 50 or higher on the area that has been treated and wear a hat. Do not use perfume of aftershave on your skin during treatment and for 4 weeks after treatment. Do not use makeup in the area that is being treated.
If you have a beard or moustache you may be required to remove it before your mask is made. During your treatment, you are advised to avoid wet shaving and use an electric razor.
Hair loss
Hair roots directly within the treatment area will be damaged by radiotherapy causing the hair to fall out. This hair loss is usually temporary and it will grow back; however it may not be as thick as before. The time it takes and the way it grows back depends on the dose of radiotherapy you have received.
Hearing problems
If your ear is included in the treated area your hearing may be affected by the treatment. This is due to swelling inside your ear and will return to normal a few weeks after your treatment has finished. Inside the ear may feel dry, sore and/or itchy. This is a normal reaction, which will settle down after treatment is finished.
Appearance
During treatment and for a short period afterwards, your appearance may be affected. The skin mimics a severe sunburn appearance, which can be difficult to conceal when treating the face and neck. However, following treatment the skin will heal with no permanent disfigurement.
Hair loss in the treated area can be very distressing, as it is important to everyone’s appearance and self-image. Hair directly within the treatment area will fall out so your appearance will be affected if you have a beard.
WHO WILL LOOK AFTER ME DURING MY TREATMENT?
Your oncologist will see you every week and at the end of your treatment, and will be the one in the overall charge of your care.
Other members of the team include:
- The Oncology Social Workers will provide guidance and assistance during your treatment and they can provide advice on financial issues;
- The Oncology nurses will provide support and check every week your weight and vital signs;
- The Radiographers who are specifically trained to deliver the radiotherapy;
- The Dietician/Medical Nutritionist will assess your nutritional wellbeing before, during and after your treatment, design an individual meal plan based on your nutritional needs, provide nutritional counselling on your current diet, make necessary adjustments to your meal plan such as food texture and ways to ease symptoms, and lastly can provide you with strategies to maintain your weight;
- The Speech and Language Therapist will provide advice and assistance with swallowing, speech and communication issues that arise from the radiotherapy you receive;
- The Pain specialist will provide you with advice and treatment options to control pain;
- The Clinical Psychologist can provide counselling about anxieties, mood swings, self-image, and provide support to you and your family during and after the treatment.



