“I have been examined and treated at many domestic and foreign hospitals, but I was most satisfied by the care I received at FV,” shared 68-year-old patient D.K.T., who lives in Ho Chi Minh City. Dr Bui Nhuan Quy, Head of FV’s Gastroenterology and Hepatology Department, successfully performed his stent replacement and gallstone removal by endoscopic retrograde cholangiopancreatography (ERCP).
Four years ago, Mr T. underwent a liver transplant surgery abroad, had a biliary stent placed and needed to be monitored periodically to determine whether the stent needed replacing. The last time Mr T. had his stent replaced was around one year ago. Due to the epidemic, the patient didn’t visit the hospital for follow-up visits and did not have his stent replaced on time. The stent became ineffective and unable to drain bile, causing blockages and infection.
When he was admitted to FV Hospital, Mr T. had symptoms of biliary tract infection, including jaundice, itching all over the body and intermittent fever and chills. At this time, Dr Quy assigned the patient to have MRI scans to confirm the diagnosis and the results showed that there was a stent in the dilated bile duct but no stones were found in the biliary tract. The patient was assigned endoscopic retrograde cholangiopancreatography (ERCP) to accurately diagnose the cause and intervene to drain the trapped bile.
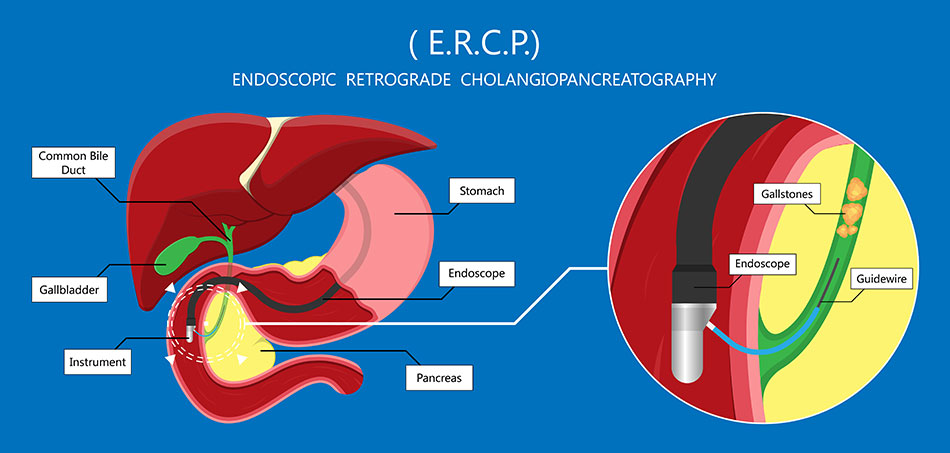
Endoscopic illustration by ERCP technique
The patient was admitted to the hospital for endoscopic retrograde cholangiopancreatography (ERCP), which combines X-ray and endoscopy to diagnose and treat problems in the liver, gallbladder, bile ducts, and pancreas.
The endoscope was inserted into Mr T.’s mouth, through the oesophagus, stomach, and then to the duodenal papilla, where the bile duct joins the duodenum. A thin plastic catheter was inserted into the bronchoscope to go to the tip of the tube and was then inserted into the duodenal papilla and bile duct to remove the old stent, found and took out six stones measuring 0.5 cm to 1 cm in size. Although the stones were removed, the bile duct was still not clear, so the doctor placed a new stent to drain the bile. The procedure ended after one hour and Mr T. was discharged after two days. After one week of follow-up examinations, he was experiencing less itching and was less jaundiced. These symptoms also completely disappeared after two weeks.
Mr T.’s daughter shared, “After listening to Dr Quy, I knew that my father needs to have his bile duct replaced periodically so that he doesn’t develop another infection.” At this time, Mr T., who was sitting nearby also shared, “I have been to many hospitals and received endoscopy by many doctors. But here, Dr Quy was so careful and gentle that when I woke up, I felt no pain and didn’t feel like I had just had surgery. I thank Dr Quy very much.”

Dr Bui Nhuan Quy and his team perform endoscopic surgery on a patient
ERCP is a modern technique which provides a high degree of accuracy in performing diagnoses and high success rate of intervention, and enables a minimally invasive stone removal procedure with few complications. This method has gradually replaced open surgery and has many advantages, including a shorter hospital stay and recovery time.
Biliary stenting is a highly advanced technique used to treat obstructions occurring in the bile ducts and requires the supervision of the treating physician who will periodically check and control the placed stent. When there are signs of increased cholestasis (reduction in bile flow), stents should be replaced, usually within three to six months, when biliary tract function will also be re-evaluated.
Because ERCP is a difficult technique, it requires an experienced and skilled physician with practice and proficiency in general gastrointestinal endoscopy skills. ERCP is only available in a few large hospitals that have developed both internal and external gastroenterology and is now being successfully applied at FV Hospital.

Dr Bui Nhuan Quy graduated from Pham Ngoc Thach Medical University in 2004 and received a Master’s degree in Internal Medicine from the University of Medicine and Pharmacy in Ho Chi Minh City in 2012. Dr Quy earned a Specialist Level II Certificate in Internal Medicine in 2021 at Pham Ngoc Thach Medical University. Dr Bui Nhuan Quy has also attended advanced training courses in his specialty, including Gastrointestinal Endoscopy (2006), Colonoscopy (2015), ERCP (2017) and attended a short-term training course in Gastroenterology at Nagoya University School of Medicine, Nagoya, Japan, in 2017.
Dr Bui Nhuan Quy is considered one of the leading gastroenterology doctors in Ho Chi Minh City and has in-depth expertise in the early diagnosis of stomach cancer, gastrointestinal endoscopy, endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic ultrasound (EUS). With 10 years of experience in the field of endoscopy and seven years in the clinical treatment of digestive diseases, Dr Quy specialises in examining and treating digestive problems and treating diseases of the stomach and duodenum, food management issues (inflammation, ulcers, polyps, cancer), colon diseases (inflammation, ulcers, polyps, irritable bowel syndrome), liver diseases (chronic hepatitis, cirrhosis, liver cancer), and diseases related to bile and gallstones. Dr Quy has successfully treated many cases with impressive results and earned the trust and respect of his patients.



