According to FV’s oncologists, around half the patients who have cancer will also develop malignant pleural effusion, of which more than 50 per cent will experience recurrent effusion, especially in terminal cases.
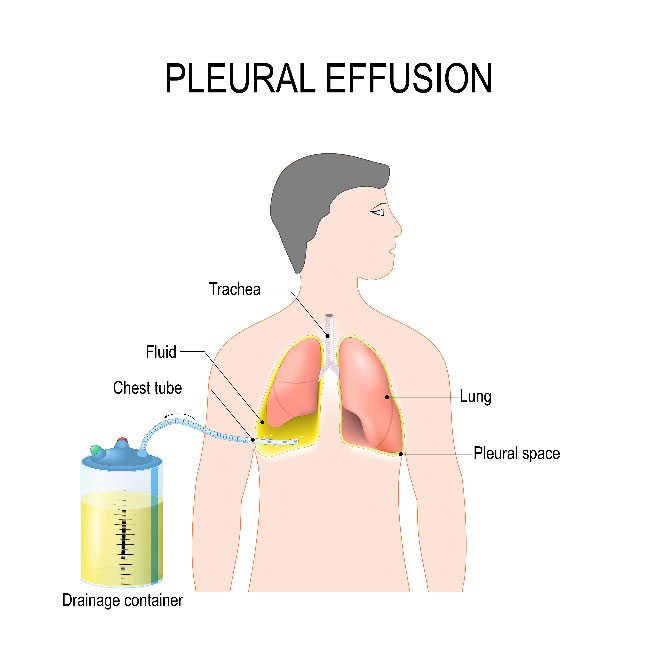
Effusion occurs when cancer cells grow in the pleural cavity (the potential space between the two visceral and parietal pleurae of the lungs), the pericardium (a thin, two-layered, fluid-filled sac that covers the outer surface of the heart), or the peritoneum, the serous membrane lining the cavity of the abdomen and covering the abdominal organs. This is a sign that cancer has spread or metastasized to other areas of the body. Common causes of pleural effusion are lymphoma and breast, lung, cervical and ovarian cancers. Recurrent pleural effusion can endanger the patient’s life or threaten the patient’s respiratory system, leading to respiratory failure, shortness of breath and angina. The fluid also recurs quickly and repeatedly performing a pleural puncture to aspirate the area many times incurs many complications, including bleeding, pneumothorax (collapsed lung) and infection.
To diagnose pleural effusion, in addition to clinical examination, the doctor will assign diagnostic tests such a chest X-ray, CT or ultrasound scan, or an ambulatory puncture.
Pleural effusion needs to be treated promptly and comprehensively so as to not endanger the patient, and improve their quality of life. The general principle of this method is to remove the pleural fluid via ultrasound-guided needle aspiration or surgical drainage of the pleural fluid, and avoid recurrence of pleural fluid by adhesion of the pleural cavity with medicine or by thoracoscopic surgery. The basic pleural puncture method has the advantages of being easy to perform, is painless and limits the duration of a hospital stay for patients. However, it also has some disadvantages, such as pneumothorax, and recurrent effusion requires intervention via puncture many times.
At FV’s Thoracic & Vascular Surgery Department, Dr Luong Ngoc Trung applies the method of drainage and pleural adhesion with medicine to prevent the regeneration of pleural fluid. This technique is performed under local anaesthesia and a small incision measuring less than one centimetre is made in the chest wall so that a drain can be inserted approximately five to six millimetres into the pleural effusion. This procedure takes around 15 minutes to perform. The pleural fluid will be drained away slowly and completely, the lung will be enlarged, and then the doctor will inject the relevant mediciation, for instance (Talc Powder, Bleomycine…) to treat the pleural space. Pleural fluid will be monitored daily until it is below 100 ml, and then the drain will be removed. Patients may stay in the hospital for around five to seven days, or they can go home and be monitored there, depending on their condition.
The advantages of this method are that it is simple, less invasive, and effective for a long time so that patients do not need to return to the hospital to have puncture very frequently. Although this method is predominantly deployed to support cancer treatment, it’s very effective in improving respiratory function and helps patients to enjoy a better quality of life. However, around 30 per cent of patients do not respond or partially respond to the above technique. In such cases, patients are required to undergo video-assisted thoracoscopic surgery (VATS).
FV Hospital is a multi-specialty hospital with a team of highly skilled and experienced doctors, equipped with modern, synchronous technologies across its various specialties. Interdisciplinary care protocols at FV Hospital are developed in consultation and with cooperation between experts in many specialties, under the supervision of the Medical Advisory Council of FV Hospital. The goal is to provide the most suitable treatment method, helping each patient to save time and costs. For example, cancer patients will be cared for by a diverse team between many specialties and/or Hy Vong Cancer Care Centre and The Pain Control Clinic, when necessary to provide additional cancer pain control and psychological support for patients.



