What is cervical cancer?
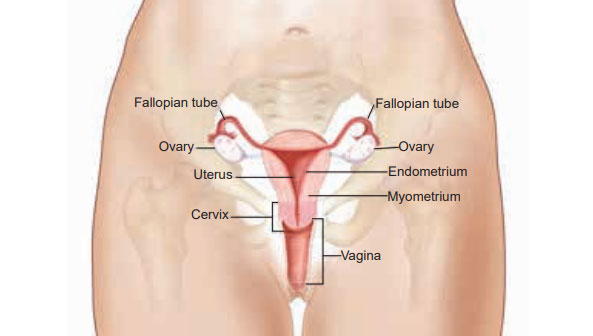
Cervical cancer is a type of cancer that occurs in the cells of the cervix — the lower part of the uterus that connects to the vagina.
Cervical cancer can affect women of all ages, but is most common in women in their 40s and 50s, although in rare cases can occur in women under 25.
Various strains of the human papillomavirus (HPV) play a role in causing most cervical cancer. HPV is a group of viruses, of which there are more than 100 different types. It is spread during sexual intercourse and other types of sexual activity (such as skin-to-skin contact of the genital areas). Most women will contract HPV at some stage during their life, but this usually clears up on its own. In a small group of women, however, the virus survives for years, contributing to the process that causes some cells on the surface of the cervix to become cancer cells.
You can reduce your risk of developing cervical cancer by having screening tests and receiving a vaccine that protects against HPV infection. Note that there is no treatment for HPV.
What are the symptoms of cervical cancer?
Early-stage cervical cancer generally produces no signs or symptoms. Some women do not experience any signs of cervical cancer at all. This is why it’s very important that you attend all of your cervical screening appointments.
Symptoms of more-advanced cervical cancer include:
- Vaginal bleeding after intercourse, between periods or after menopause;
- Watery, bloody vaginal discharge that may be heavy and have a foul odour;
- Pelvic pain or pain during intercourse.
The vast majority of women with the symptoms listed above do not have cervical cancer, and are far more likely to be experiencing other conditions, such as infections.
What increases my risk of cervical cancer?
The fact that HPV infection is very common but cervical cancer is relatively uncommon suggests that only a very small proportion of women are vulnerable to the effects of an HPV infection. There appear to be additional risk factors that affect a woman’s chance of developing cancer of the cervix. These include:
- Smoking – women who smoke are twice as likely to develop cervical cancer as women who don’t; this may be caused by the harmful effects of chemicals found in tobacco on the cells of the cervix;
- Immunosuppression drugs – women who are on immunosuppression drugs (reduces the strength of the body’s immune system) can be at increased risk of developing cervical cancer.
How can I reduce my risk of cervical cancer?
- Get vaccinated against HPV: the HPV vaccine protects girls from developing cervical cancer when they are adults. This is why the HPV vaccine is offered to all girls from 9 to 26 year-old to protect them from cervical cancer in adulthood. The vaccine is most effective if given to girls before they become sexually active.
- Don’t smoke.
- Have routine Pap tests (cervical cytology screening, also called smear tests): during a Pap test, your doctor scrapes and brushes cells from your cervix, which are then examined in a lab for abnormalities. A Pap test can detect abnormal cells in the cervix, including cancer cells and cells that show changes that increase the risk of cervical cancer.
- HPV DNA test: this test involves testing cells collected from the cervix for infection with any of the types of HPV that are most likely to lead to cervical cancer.
FV Hospital offers cervical cancer screening based on the guidelines from the American Congress of Obstetricians and Gynaecologists:
- Cervical cancer screening should begin at age 21 years;
- Pap test is recommended every 3 years for women between the ages of 21 and 29 years;
- For women aged 30-65 years, co-testing with Pap test and HPV DNA test is preferred and should be performed every 5 years.
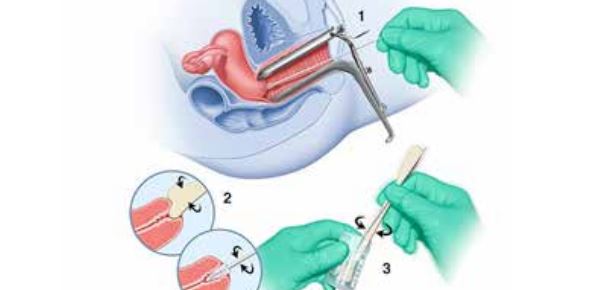
Pap Test
How is cervical cancer diagnosed?
If cervical cancer is suspected, your doctor is likely to start with a thorough examination of your cervix. A special magnifying instrument (colposcope) is used to check for abnormal cells.
During the colposcopic examination, your doctor is likely to take a sample of cervical cells (biopsy) for laboratory testing. To obtain tissue, your doctor may use:
- Punch biopsy, which involves using a sharp tool to pinch off small samples of cervical tissue;
- Endocervical curettage, which uses a small, spoon-shaped instrument (curet) or a thin brush to scrape a tissue sample from the cervix.
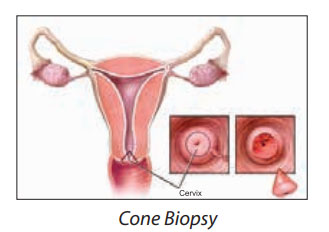
If the punch biopsy or endocervical curettage is worrisome, your doctor may perform a cone biopsy, which is a procedure done in the hospital under general anaesthesia, that allows your doctor to obtain deeper layers of cervical cells for laboratory testing.
How is cervical cancer treated?
Treatment for cervical cancer depends on several factors, such as the stage of the cancer, other health problems you may have and your preferences. Surgery, radiation, chemotherapy or a combination of the three may be used.
Early-stage cervical cancer is typically treated with surgery to remove the uterus (hysterectomy). A hysterectomy can cure early-stage cervical cancer and prevent recurrence. Minimally invasive surgery may be an option for early-stage cervical cancer.
Radiotherapy may be used alone or with chemotherapy before surgery to shrink a tumour or after surgery to kill any remaining cancer cells.
What if abnormal cells are found during screening?
If your screening results show that you don’t have cancer of the cervix, but there are biological changes that could turn cancerous in the future, your surgeon will usually remove the abnormal cells under anaesthesia by performing a cone biopsy (the area of abnormal tissue, in the shape of a cone, is removed during surgery).



