WHAT IS A NEEDLE BIOPSY OF THE LUNG?
Chest radiography and chest CT scanner reveal many abnormalities but often, the image is not sufficient to confirm the diagnosis. Taking a sample with a needle under CT guidance allows a microscopic examination, and the result will provide more information on the diagnosis.
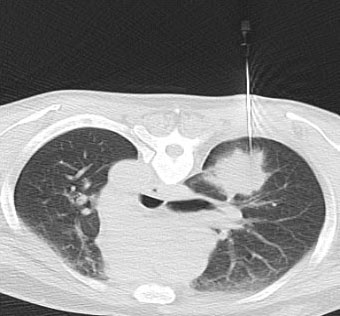
A CT-guided trans-thoracic needle biopsy involves introducing a needle through the thorax under the guidance of CT scanner to remove some tissue from the nodule and examining it under a microscope to determine a diagnosis.
In many cases the lesion is a nodule. Although more than half of single (called solitary) lung nodules are benign, some can be cancerous.
When a doctor orders a trans-thoracic biopsy, the diagnosis is usually believed to be unreachable by other diagnostic techniques, such as bronchoscopy, cytology, blood analysis.
HOW SHOULD I PREPARE?
You will be instructed to avoid eating or drinking for 4 hours before your biopsy. However, you may take your routine medications with sips of water.
Prior to a needle biopsy, you should report to your doctor all medications that you are taking, and if you have any allergies, especially to anaesthesia drugs. Your doctor will advise you to stop taking aspirin or a blood thinner at least 3 days before your procedure.
Also, inform your doctor about recent illnesses or other medical conditions.
You will be asked to fill out a questionnaire and a consent form prior to the procedure.
You may be asked to remove some or all of your clothes and to wear a gown during the procedure. You will also be asked to remove jewellery and any metal objects or clothing that might interfere with the X-ray transmission.
Women should always inform their doctor or diagnostic radiographer if there is any possibility that they are pregnant. Many imaging tests are not performed during pregnancy so as not to expose the foetus to radiation. If an X-ray is necessary, precautions will be taken to minimise radiation exposure to the baby.
It is recommended to have a relative or friend accompany you and drive you back home afterward.
HOW IS THE PROCEDURE PERFORMED?
Imaging-guided, minimally invasive procedures such needle biopsy of the lung are most often performed by a specially trained interventional radiologist.
CT-guided needle biopsies of the lung are usually done on an inpatient basis.
A limited CT scan will be performed to confirm the location of the nodule and the safest approach. Once the location of the nodule is confirmed, the entry site is marked on the skin. The skin around the insertion site will be cleaned and disinfected, and a sterile drape with a holed centre will be applied.
A local anaesthesia will be injected to numb the entry site.
CT-guided biopsies require patients to be able to hold still on the CT table for up to 30 minutes.
A very small nick is made in the skin at the site where the biopsy needle is to be inserted.
Under CT guidance, the radiologist will insert the needle at the site already marked and advance it directly into the nodule. As tissue samples are taken, you may hear clicks from the sampling instrument. After this sampling, the needle will be removed. Tissue samples will then be removed from the needle.
This process may be repeated 1 or 2 times.
Once the biopsy is complete, pressure will be applied to stop any bleeding and the opening in the skin is covered with a dressing.
This procedure is usually completed within an hour.
You will be taken to an observation area for at least 6 hours. X-ray(s) or other imaging tests may be performed to monitor for complications.
WHAT WILL I EXPERIENCE DURING AND AFTER THE PROCEDURE?
When you receive the local anaesthetic to numb the skin, you will feel a slight pin prick from the needle. You may feel some pressure when the biopsy needle is inserted. The area will become numb within a short time.
You will be asked to remain still and not to cough during the procedure. You also will be asked to hold your breath multiple times in the same position during the biopsy. It is important that you try to maintain the same breath-hold each time to insure proper needle placement, as the nodule is moving when breathing.
Usually, your dressing will be removed 1 day following the procedure and you may bath or shower as normal.
You should not exert yourself physically (such as heavy lifting, extensive stair climbing, sports, etc.) the night of and for 1 full day following your biopsy. On the second day, if you feel up to it, you may return to your normal activities. For the next 10 days, you should avoid intense physical exercise.
You may experience some soreness at the biopsy site as the local anaesthesia fades, but this should improve. You may also cough up a little blood, but this should be minimal.
These symptoms will gradually fade over the 12 to 48 hours following the procedure.
If you feel pain or breathing discomfort, please contact your doctor immediately or come to the Accident and Emergency department.
WHO INTERPRETS THE RESULTS AND HOW DO I GET THEM?
A pathologist examines the removed specimen and attempt to make the diagnosis so that treatment planning can begin. Be aware that it is not always possible to obtain a diagnosis from the sample and if no diagnosis can be reached other diagnostic methods may be discussed with you by your doctor
WHAT ARE THE BENEFITS VERSUS RISKS?
Benefits
Needle biopsy is a reliable method of obtaining tissue samples that can help diagnose whether a nodule is benign or malignant.
A needle biopsy is less invasive than surgical biopsies which often involve a larger incision in the skin and general anaesthesia.
Generally, the procedure is not painful and the results are as accurate as when a tissue sample is removed surgically.
Recovery time is brief and patients can soon resume their usual activities.
Risks
Any procedure where the skin is penetrated carries a risk of infection. The chance of infection requiring antibiotic treatment appears to be less than one in 1,000 cases.
Bleeding at the entry site is rare, but coughing up blood can occur.
An air leak from the punctured lung into the pleural cavity surrounding the lung may occur. This situation is called pneumothorax and may lead to lung collapse. Signs of a collapsed lung include shortness of breath, difficulty in catching your breath, rapid pulse, sharp chest or shoulder pain with breathing. In most cases, the pneumothorax disappears spontaneously. If the pneumothorax is large enough to be considered harmful, a small tube may be inserted into the chest cavity to drain away the air. This tube is generally removed within a few days.
Bleeding from the punctured lung into the pleural cavity may eventually cause your lung to collapse as the blood pushes on the outside of the lung. This situation is called haemothorax and it requires the insertion of a surgical chest drain, to evacuate the blood from the pleural cavity.
For further information, kindly contact our Imaging department at (028) 54 11 34 00



